Early detection of Coronary Heart Disease and Coronary Artery Disease is crucial in preventing death from these conditions. This article describes the various tests undertaken to diagnose heart disease and will be of help to anyone who has experienced chest pains and is unsure of the next step to take.
Contents
- Introduction
- Diagnosing the type of chest pain and other usual symptoms
- Diagnosing Coronary Heart Disease with the latest technology
Introduction
Coronary artery disease (CAD) remains the leading cause of death and morbidity in the United Kingdom, killing more than 90,000 people each year. The most common symptom of coronary artery disease is chest pain. The lifetime risk of developing coronary artery disease in the UK by the age of 40 has been estimated at 50% in men and 33% in women and every year around one in five men, and one in six women will die from CAD. There have been tremendous improvements in our knowledge of the underlying process of heart disease but unfortunately 30% of people who have a heart attack will not survive. This means that early detection of the condition is critically important.
Diagnosing the type of chest pain and other usual symptoms
It is important to obtain an accurate and rapid diagnosis of coronary artery disease at the outset as there may be serious consequences with a missed diagnosis; this is also important to exclude chest pain that is not related to the heart. It is extremely important to understand that the symptoms of heart disease are different in men and women, and also in different ethnic groups. Women generally have heart attacks later in life (over the age of 55), their symptoms are often masked and may be quite different from the typical angina pain experienced by men. A normal electrocardiogram (ECG) does not always exclude a heart attack or angina. Similar problems are faced in diabetic patients, where the disease may remain “silent” for many years (1). Chest pains are often the first tell-tale signs of coronary heart disease; however, in many instances the exact cause of chest pain can remain elusive, leading to a large number of ‘false’ diagnoses.
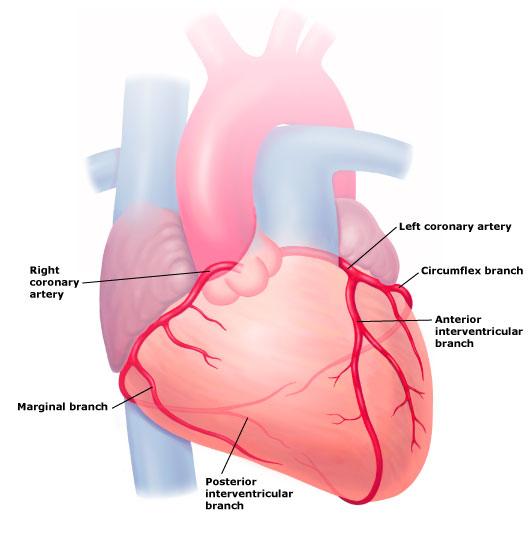
Coronary Artery Disease (CAD)
Blood supply to our heart is provided by blood vessels called coronary arteries. There are three main coronary arteries namely Right Coronary Artery (RCA), Left Anterior Descending artery (LAD) and Left Circumflex artery (LCx). These arteries can become narrowed due to cholesterol deposits and this process is called atherosclerosis. Greater cholesterol-like ‘fatty’ build-up in the arteries may often cause a reduction of blood delivery to the heart muscle, leading to chest pain, which is termed ‘angina’. A heart attack or ‘myocardial infarction’occurs when a small portion of the deposited cholesterol in the wall of the heart arteries (coronary arteries) breaks off (atherosclerotic plaque rupture). A blood clot can form around this rupture causing a sudden reduction in blood flow to the heart muscle often resulting in a heart attack.
The key features which make a diagnosis of angina likely are when:
- Pain is localised to chest and/or radiating to neck, jaw, left arm and shoulder
- Chest pain is worse on exercise and during stress
- Chest pain is relieved by rest and/or by nitroglycerine tablet or spray
These symptoms do not always occur in everyone. Some patients may describe only arm or jaw pain, or angina may present as indigestion or chest tightness. Stable angina is brought on by physical activity or stress in a reproducible manner. Unstable angina denotes an increase in the frequency of chest pain even with low level of activities or when symptoms occur at rest. If a sudden change occurs in a previously stable patient, then the patient should be urgently reviewed by a doctor or hospital. Recent NICE (National Institute for Health and Clinical Excellence) guidelines recommend the following for those with stable chest pain:
For patients with a low likelihood of coronary artery disease (young patients, non-smokers, patients with no history of diabetes or high cholesterol) a coronary calcium scan should be used as a first line investigation. Functional imaging (myocardial perfusion scan to look at heart blood flow) has been recommended for patients with intermediate risk. An invasive coronary angiogram is recommended for patients in high risk group only.
Tests for detecting Coronary Heart Disease (CHD)
Electrocardiography/Exercise ECG
Electrocardiography (ECG) is the first test, and it records the electrical activity of the heart. It is painless and harmless and takes only a few minutes. The exercise ECG entails leads being attached to the chest that measure how the heart functions whilst exercising, either on a treadmill or an exercise bicycle. Though widely used, the diagnostic accuracy has been called into question, thus the new NICE Guidelines for chest pain have evolved. The use of an exercise test alone led to many false positive tests leading to unnecessary, expensive, and invasive coronary angiography, where nearly 50% of the tests were normal. However, in good hands, an exercise test remains a very useful investigation.
Non-invasive Coronary Angiography by Computed Tomography (CTCA)
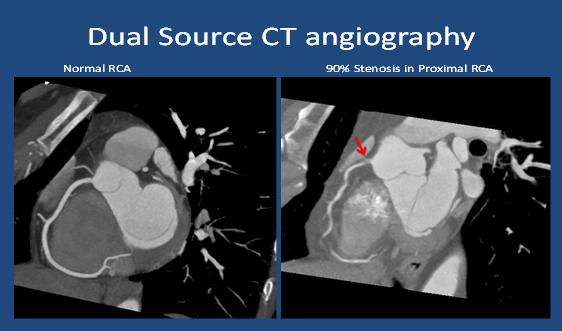
Non-invasive coronary angiography by computed tomography (CTCA) is a new and evolving technique which can accurately image/detect the presence of coronary artery disease (atherosclerosis) inside the heart arteries. Imaging of the heart is a technically challenging task because of its continuous motion during the heartbeat. Traditional CT scanners are inadequate, but there has been considerable improvement in CT technology. The ultrafast dual-source CTCA requires only a few seconds to image the heart arteries accurately with low, and acceptable levels of radiation exposure. CTCA has gained clinical acceptance for the accurate non-invasive diagnosis of CAD (2). Click on image to enlarge.
Acute chest pain syndrome is a relatively common condition and diagnosis is often difficult and expensive. Recent trials have demonstrated that CTCA allows for rapid and accurate diagnosis. CTCA is also able to identify nearly three times as many patients with CAD as the standard traditional methods.Guidelines from the American College of Cardiology Foundation (ACCF) and American Heart Association (AHA) recommend use of CTCA in patients presenting with acute chest pain.
The whole procedure takes around 30 minutes. A contrast agent will be given via an intravenous line (IV) to help produce the images. It is common to feel a warm sensation as the contrast agent circulates through the body. The new generation CT scanners provide excellent and accurate diagnosis of CAD with acceptably low radiation (3). A non-contrast “calcium score” can be also performed and this can be used as a screening test. The higher the calcium score, the higher the risk of having heart attack. A calcium score of zero is associated with a very low risk of major heart attack over the next 3–5 years (4).
Benefits of Dual-Source Cardiac CT Imaging
- Imaging time is 15 seconds, total procedure time is 30 minutes
- Allows early detection of heart disease and improved prognosis due to earlier treatment
- Is able to pick up "silent" disease, which is important in diabetic patients
- Can diagnose the extent and progression of heart disease
- Can conclusively rule-out cardiac disease in those cases with non-cardiac chest pain
- Is non-invasive and a low risk procedure
Myocardial perfusion scans (MPS)
A myocardial perfusion scan can check how well blood is flowing to the heart muscle. This is an established and validated technique for the non-invasive and accuratediagnosis of the severity of coronary artery disease and risk of heart attack (5). The diagnostic accuracy is improved with MPS heart scans. An MPS heart scan involves a safe and very small amount of radioactive substance being injected into the body, this concentrates in the heart muscle and can be viewed using special ‘gamma’ cameras. MPS has the disadvantage of being a resource-intensive test and requires considerable infrastructure and skilled staff, thereby restricting the scan to limited centres of excellence in the UK. MPS is a well-established test and it provides important prognostic information to stratify the risk to cardiac patients. Though MPS accurately predicts the severity of obstructed coronary arteries, it does not directly image the heart arteries as can be done now by new and evolving CTCA cardiac technology.
Stress Echocardiogram
This is a non-invasive test and it can be done at the bedside. This scan uses sound waves to build up a moving picture of the heart whilst both at rest and under stress when exercising. It can provide helpful information, including the size and shape of the heart, pumping capacity and the location and extent of any tissue damage. Also it helps to evaluate heart valves. However this test is also limited by the shortage of skilled personnel and there are technical difficulties that restrict its accuracy and usefulness in the detection of coronary artery disease.
Invasive Coronary Angiogram
This is the classical “gold standard” for imaging the coronary arteries. Thisis an invasive test where a narrowcatheter is inserted into an artery in the arm or groin and is directed through the vessel into the coronary arteries. A contrast dye is injected which enables the coronary arteries to be visualised on an x-ray machine. Though this test is ultimately required for treatment purposes, such as angioplasty (balloon) and stent insertion used to dilate blocked arteries, this test is now rarely required as a purely diagnostic test. Significant complicationssuch as bleeding, myocardial infarction and stroke can occur, although these are rare.
Diagnosing Coronary Heart Disease with the latest technology
The Cardiac Imaging and Research Centre (CIRC) is one of the specialised centres in London with the latest state-of-the-art scanners that provide rapid, accurate and early diagnosis of heart disease. The department is attended by highly skilled cardiologists and also a comprehensive multi-disciplinary team who provide the highest quality of heart tests.
CIRC is unique in that it is also supported by the British Cardiac Research Trustand is acknowledged for the outstanding quality of clinical research and training that it undertakes. Key research and important clinical trials are performed by BCRT at CIRC. Please see the website for further details: www.britishcardiacresearch.org.
In conclusion, it is of immense importance when treating suspected heart disease to have rapid and conclusive diagnosis and we now have the technology to facilitate this.
References
1. Anand DV, Lim E, Hopkins D, Corder R, Shaw LJ, Sharp P, Lipkin D, Lahiri A.Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calciumimaging and selective myocardial perfusion scintigraphy. European Heart Journal 2006;27(6):713-721
2. Samad Z, Hakeem A, Mahmood SS, Pieper K, Patel MR, Simel DL, Douglas PS. A meta-analysis and systematic review of computed tomography angiography as a diagnostic triage tool for patients with chest pain presenting to the emergency department. Journal of Nuclear Cardiology 2012;19(2):364-376
3. Venuraju S, Yerramasu A, Lahiri A. Advances in cardiac computed tomography: An update for primary physicians. Primary Care Cardiovascular Journal 2009;2:131-137
4. Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing committee to update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and Society of Cardiovascular Computed Tomography. Journal of the American College of Cardiology 2007;49(3):378-402
5. Sabharwal NK, Lahiri A. Role of myocardial perfusion imagingfor risk stratification in suspected or known coronary artery disease. Heart 2003;89(11):1291-1297









