Arteriovenous malformations are a relatively rare vascular condition but are responsible for approximately 2% of strokes. This article discusses the risks of arteriovenous malformations alongside their diagnosis and treatment options.
Contents
- What is an arteriovenous malformation (AVM)?
- What are the symptoms caused by AVMs?
- What is the risk of bleeding caused by an AVM?
- Who is affected?
- How is a diagnosis of an AVM made?
- What treatments are available?
- Additional resources
What is an Arteriovenous Malformation (AVM)?
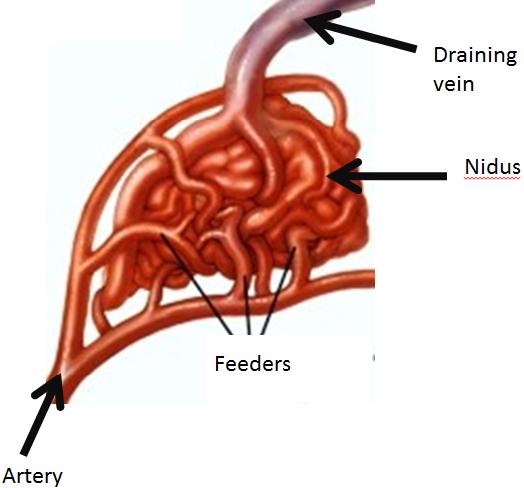 Normally blood flows from the heart to the arteries of the body. The arteries branch and get smaller until they become a capillary, which is just a single cell thick. In this way blood pressure drops to very low levels that the thinner walled veins can cope with. In an arteriovenous malformation (AVM), usually early in life, arteries connect directly to veins. This is a high-pressure shunt or fistula. Veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge and create what we call a “nidus”. Usually there are multiple feeding vessels in an AVM and many draining veins.
Normally blood flows from the heart to the arteries of the body. The arteries branch and get smaller until they become a capillary, which is just a single cell thick. In this way blood pressure drops to very low levels that the thinner walled veins can cope with. In an arteriovenous malformation (AVM), usually early in life, arteries connect directly to veins. This is a high-pressure shunt or fistula. Veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge and create what we call a “nidus”. Usually there are multiple feeding vessels in an AVM and many draining veins.
Apart from the typical AVM described above there are other “vessel abnormalities” routinely seen in scans of the brain (Venous malformation – abnormal cluster of enlarged veins resembling the spokes of a wheel with no feeding arteries; low pressure, rarely bleed and usually not treated and Capillary telangiectasia – abnormal capillaries with enlarged areas; very low pressure and usually not treated as well).
AVMs can occur anywhere in the brain and spinal cord. Brain AVMs can occur on the surface (also called cortical), deep (in the thalamus, basal ganglia, or brainstem), and within the dura (the tough protective covering of the brain). Spinal AVMs can occur on the surface (extramedullary) or within the spinal cord (intramedullary).
What are the symptoms?
The symptoms of AVMs vary depending on their type and location. While migraine-like headaches and seizures are general symptoms, most AVMs do not show symptoms (asymptomatic) until a bleed occurs. Common signs of brain AVMs are:
• Sudden onset of a severe headache, vomiting, stiff neck.
• Seizures.
• Migraine-like headaches.
• Swelling or redness of an eye in people with a particular type of dural AVM called a carotid-cavernous fistula.
• Noise in the head, called a "bruit”. A dural AVM can cause a bruit due to the blood flowing through it.
AVMs can damage the brain or spinal cord in three basic ways:
1. AVMs can rupture and bleed into the brain—called an intracerebral haemorrhage (ICH), or it can bleed into the space between the brain and skull—called a subarachnoid haemorrhage (SAH). Bleeding is the most serious complication of a vascular malformation, because of the risk of brain damage and so it is treated as an emergency. Sometimes a bleed may be small and produce no symptoms at all.
2. AVMs can grow large and create pressure against the surrounding brain, resulting in seizures and hydrocephalus. This is more common in large AVMs.
3. AVMs can reduce the amount of oxygen delivered to nearby tissues. Because the blood flows directly from the artery to the vein, cells that normally get oxygen from the capillaries begin to deteriorate.
What is the risk of bleeding?
The risk of AVM bleeding is 2 to 3% per year. Death from the first haemorrhage is between 10 to 15%. Once a haemorrhage has occurred, the AVM is more likely to bleed again during the first year (6%). Life time risk is more difficult to calculate in particular for incidental, non ruptured AVMs. For example, a 25-year-old man has an 80% lifetime risk of bleeding (at least once). Many factors affect this percentage, including where the AVM is located and what type of AVM it is. It's best to talk to your doctor about your own individual risk.
Who is affected?
AVMs of the brain and spine are congenital (present at birth) and relatively rare. They affect both men and women at about the same rate. They can occur at all ages, but most often cause symptoms between 20 and 40 years of age. AVMs account for about 2% of all haemorrhagic strokes each year.
How is a diagnosis made?
Whether you or your loved one was brought to the emergency room with a ruptured AVM or are considering treatment options for an unruptured AVM, the doctors will learn as much as possible about your symptoms, current and previous medical problems, current medications, family history, and they will perform a physical exam. Diagnostic tests are used to help determine the AVM's location, size, type, and involvement with other structures.
• Computerized Tomography (CT) scan is a non-invasive x-ray to view the anatomical structures within the brain to detect blood in or around the brain. A newer technology called CT angiography involves the injection of contrast into the blood stream to view the arteries of the brain. This type of test provides the best pictures of blood vessels through angiography and soft tissues through CT.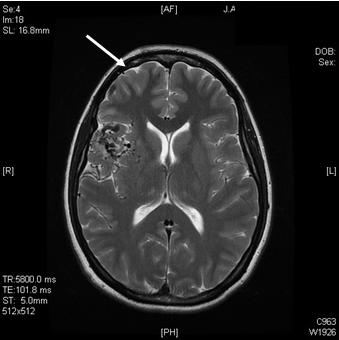
• Magnetic Resonance Imaging (MRI) scan is a non-invasive test, which uses a magnetic field to give a detailed view of the soft tissues of your brain. An MRA (Magnetic Resonance Angiogram) is the same non-invasive study, except it is also an angiogram, which means it also examines the blood vessels, as well as the structures of the brain.
• Angiogram is an invasive procedure, where a catheter is inserted into an artery 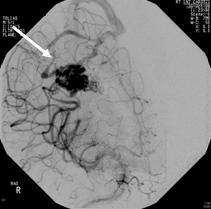 and passed through the blood vessels to the brain. Once the catheter is in place, a contrast dye is injected into the bloodstream and the x-ray images are taken.
and passed through the blood vessels to the brain. Once the catheter is in place, a contrast dye is injected into the bloodstream and the x-ray images are taken.
What treatments are available?
Surgery, endovascular therapy, and radiosurgery can be used alone or in combination to treat an AVM. Endovascular embolisation is often performed before surgery to reduce the AVM size and risk of operative bleeding. Radiosurgery or embolisation may be used after surgery to treat any remaining portions of the AVM. Your neurosurgeon will discuss all the options with you and recommend a treatment that is best for your individual case.
Observation
If there have been no previous haemorrhages, the doctor may decide to observe the patient, which may include using anti-convulsants to prevent seizures and medication to lower blood pressure.
Radiosurgery
Radiosurgery aims a precisely focused beam of radiation at the abnormal vessels. The procedure takes several hours of preparation and one hour to deliver the radiation. The patient goes home the same day. After six months to two years, the vessels gradually close off and are replaced by scar tissue. The advantages of this treatment are that there is no incision and the procedure is painless. The disadvantages are that it works best with smaller AVMs and may take a long time to show effect (during which time risk of haemorrhage exists). Treatment can be delivered by either Gamma Knife® or CyberKnife®.


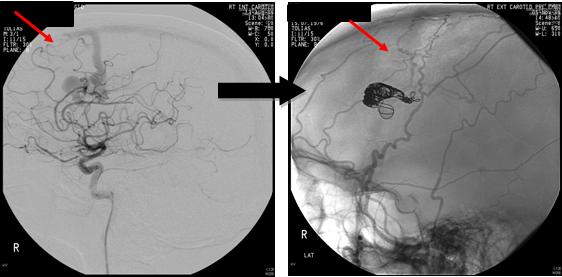
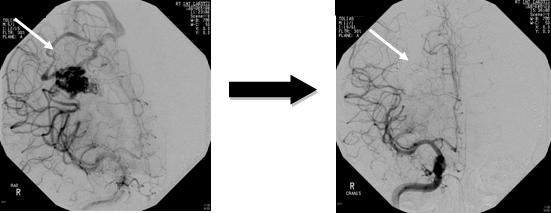
Endovascular therapy
Endovascular treatment uses small catheters inserted into your blood vessels to deliver glue or other obstructive materials into the AVM so that blood no longer flows through the malformation. It is performed in the angiography suites of a radiology department by a neuroradiologist. The procedure is performed under general anaesthesia. A small incision is made in the groin and a catheter is inserted into an artery then passed through the blood vessels to the feeding arteries of the AVM. Occluding material, either coil or acrylic glue, is passed through the catheter into the AVM. The procedure time can vary, and the patient remains in the hospital for several days for observation. The advantage of this treatment is it's less invasive than surgery and can be used to treat deep or inoperable AVMs. Disadvantages include risk of embolic stroke from the catheter and rebleeding since the AVM is not completely obliterated. Multiple treatments may be necessary.
Surgery
Using general anaesthesia, a surgical opening is made in the skull, called a craniotomy. The brain is gently retracted so that the AVM may be located. Using a variety of techniques such as electrocautery, the AVM is shrunk and dissected from normal brain tissue. The type of craniotomy performed depends on the size and location of the AVM. The option of surgery also depends on the general health of the patient. The advantage of surgical treatment is that a cure is immediate if all the AVM is removed. Disadvantages include risk of bleeding, damage to nearby brain tissue, and stroke to other areas of the brain once removed.
Additional resources
• Brain and Spine Helpline (Information and support on neurological disorders for patients, carers and health professionals)
• Brain and Spinal Injury Charity (BASIC) (Information, research and support groups)
• British Epilepsy Association (Information and advice)
• Chest, Heart and Stroke Scotland (Advice, information, education and research in Scotland)
• Crossroads (Practical support for carers and respite care at home)
• Different Strokes (Support for younger stroke survivors)
• DVLA Drivers’ Medical Group 01792 783686; (Fitness to drive)
• Epilepsy Association of Scotland (Information and advice helpline)
• Migraine Trust (Research, training, information and support)
• National Society for Epilepsy (Medical support, counselling and information)
• Speakability (Advice and support for people affected by aphasia)
• Stroke Association (Information, support and publications)
An AVM or arteriovenous malformation forms when arteries connect directly to veins. This direct connection forms a high-pressure shunt or fistula. The veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge to create a “nidus”. Usually there are multiple feeding vessels in an AVM and many draining veins.
Full medical glossaryAn AVM or arteriovenous malformation forms when arteries connect directly to veins. This direct connection forms a high-pressure shunt or fistula. The veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge to create a “nidus”. Usually there are multiple feeding vessels in an AVM and many draining veins.
Full medical glossaryAssociated with the nervous system and the brain.
Full medical glossary





