A comprehensive overview of the variety of ways in which the latest neurosurgery treatments can be used to treat epilepsy, movement disorders and pain.
The Expert Guide to Neurosugery: Including latest treatments for:
- Epilepsy,
- Movement Disorders and Pain - including Trigeminal Neuralgia
- Brain Haemorrhage,
- Cerebral Aneurisms and
- Arteriovenous Malformations (AVMs)
Contents
- Comprehensive epilepsy care
- Functional neurosurgery
- Movement disorders
- Pain
- Paediatrics
- Brain haemorrhage
- Cerebral Aneurysms
- Arteriovenous malformations (AVMs)
The aim of neurosurgery has always been to gain the maximum benefit for the patient with the minimum amount of risk.
Modern neurosurgery achieves this aim in three ways:
- Start with the least invasive treatment possible and move to more invasive treatments as required.
- Work in a team to ensure the patient benefits from the widest range of informed opinion before deciding on a treatment plan – these multidisciplinary teams always include more than one neurosurgeon and other related specialists e.g. radiologists, oncologists, physiotherapists etc. The patient and their family are part of the team as any treatment decisions must recognise that their wishes are paramount. The surgeons involved in the team should not only be fully trained neurosurgeons but super-specialists in that particular area of neurosurgery e.g. neurosurgeons with particular training in brain tumours or paediatric neurosurgery etc.
- The use of modern technology such as gamma knife.
Of these three principles the first two are by far and away the most important. It is important to bear these principles in mind as we discuss the different types of modern neurosurgical treatments available.
Comprehensive epilepsy care
Epilepsy is a common disorder affecting about one in two hundred people of all ages. In the majority, drug treatment will provide good control of the seizures but in at least 10% ongoing attacks occur despite trying several drugs (refractory seizures). In this case it is often appropriate to consider epilepsy surgery.
Most refractory seizures arise from a single focus (location) within the brain and it is frequently possible to identify this region in an individual. Often the area is not functioning correctly and removal can abolish the seizures without affecting normal functions. If this is not possible then there are a variety of electrical stimulation techniques which allow for much improved seizure control without the need for removing tissue. Vagus nerve stimulation, for example, offers treatment, often without the need even for an overnight stay in hospital which in many cases will improve control substantially.
The treatment of epilepsy is complex and it is important that all aspects of the condition are considered. Top quality comprehensive epilepsy care requires a specialist team including neurologists, neurophysiologists, radiologists and surgeons to ensure optimum control and quality of life is achieved for every individual.
Functional neurosurgery
Functional neurosurgery is the name given to the treatment of a wide variety of neurological conditions where the function of the nervous system is abnormal even though its structure remains normal. The treatments aim to restore normal function by stimulating the nervous system and unlike many other treatments are not destructive in nature. These treatments have the advantage of working when medication has failed or indeed allowing a patient to be free of the side-effects of medication which in a condition such as Parkinson’s disease can be very significant. Currently functional neurosurgery falls into two major categories: the treatment of abnormal movement (movement disorders) and the treatment of pain.
Movement disorders
The last decade has seen major progress in the treatment of advanced movement disorders such as Parkinson’s disease, essential tremor, Multiple Sclerosis tremor and dystonia. Neuromodulation in the form of deep brain stimulation is a technique which provides an effective, safe, non-destructive, adjustable and largely reversible treatment in patients with movement disorders in whom medical treatment fails to control symptoms or causes significant side effects. The treatment not only improves movements, but serves to give back the quality of life that every patient deserves.
Pain
Intractable pain remains a major burden for the patients. Recent advances in neurosurgery have allowed the development of safe and effective techniques to treat a variety of pain syndromes. Spinal cord stimulation is now an approved treatment for painful conditions such as causalgia, post herpetic pain and Failed Back Surgery Syndrome. Occipital nerve stimulation is effective for treating occipital neuralgia, cluster headaches and many types of migraine. Deep brain stimulation achieves good control for post-stroke pain and many types of facial pains. Such techniques have the added advantage of being non-destructive and largely reversible.
Trigeminal neuralgia
Trigeminal neuralgia is a relatively common condition affecting as many as 1 in 200 of the population at sometime in their life. It causes severe pain in one side of the face, usually in a specific area of the cheek or jaw. It may involve the forehead, eye and often the teeth. The pain tends suddenly to stab, like a bolt of lightening, frequently brought on by minor brushing of the face, eating or cold wind or water touching a ‘trigger point’ on the face. Pain is typically extremely severe and standard painkillers may have only a minor benefit.
Happily in most situations trigeminal neuralgia can be successfully treated and a totally pain-free outcome is the aim. Correct diagnosis is crucial, involving specialist tests including an MRI scan of the brain. The condition is frequently associated with an abnormal course of a blood vessel close to the brain pressing on the trigeminal nerve which provides sensation for the face. Many are successfully treated with a drug to reduce the aberrant firing of the nerve. If that proves ineffective, or the side effects of the medication limit the use, then there are a number of surgical treatments with excellent results. Depending on the specific case and the sufferer’s preference this can involve targeted injection under anaesthetic, up to brain surgery for the most severe cases. Focused radiation treatment using the CyberKnife® may allow successful ‘surgical’ treatment without the need for anaesthetic or penetration of the skin.
Paediatrics
This is neurosurgery in children, and requires dedicated paediatric neurosurgeons with experience of operating on the developing nervous system working in close collaboration with paediatricians to achieve the best outcome for each child. The London Neurosurgery Partnership has assembled just such a group.
Hydrocephalus
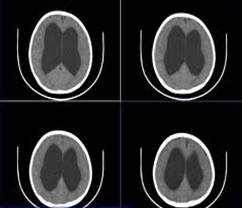
The brain and spine are hollow and contain fluid known as cerebro-spinal fluid (CSF). The cavities in the brain containing the fluid are known as ventricles. This fluid also surrounds the brain and spine. The CSF protects the brain from impact on the skull and also nourishes the brain. The adult brain produces around 500 ml of fluid per day, however the capacity for the fluid in the brain is only 125 ml. Thus the fluid is produced and circulates around the brain and then is reabsorbed into the blood. The brain keeps the situation of fluid production and re-absorption in balance so that there is a constant amount of fluid around the brain. Any mechanism which disrupts this balance can cause too much fluid within the brain. This is known as hydrocephalus. In general terms hydrocephalus can occur when too much fluid is produced, the circulation of fluid is blocked, or not enough fluid is reabsorbed into the bloodstream. This condition tends to be commoner in children because the tumours that occur in children tend to grow next to critical parts of the fluid chambers.
Brain haemorrhage
Haemorrhagic strokes are frequently caused by untreated raised blood pressure as well as the bursting of an aneurysm (an abnormal "bulging" of a blood vessel in the brain) or an arteriovenous malformation (AVM), a cluster of abnormal blood vessels. In the case of an aneurysm, the weak spot in the vessel wall can be stretched out over the years, often by high blood pressure, which ultimately causes it to rupture. While aneurysms may not cause any symptoms until they burst (sometimes causing people to liken them to "time bombs" in the brain), AVMs may have many associated symptoms including seizures, progressive neurologic problems and severe headaches that are unresponsive even to strong medications.
Until recently, some aneurysms and AVMs were virtually impossible to treat without high risk to the patient. New diagnostic and surgical advances have made it possible to treat these important causes of stroke and offer patients the likelihood of a cure.
Treatment of brain haemorrhage
Treatment may involve carefully controlling blood pressure, which can be too high or too low, using medication to control brain swelling and sometimes, surgery is needed to save the patient's life or to improve the chances of recovery. The type of surgery depends upon the specific cause of brain bleeding. For example, a haemorrhage due to an aneurysm or AVM requires special treatment.
Cerebral Aneurysms
Aneurysms are weaknesses in the wall of the cerebral blood vessels that develop over time. We do not know what causes a cerebral aneurysm formation, but most studies suggest that they occur in between 2% and 5% of the whole population. Because these areas are abnormal they have a risk of rupture (“bursting”) that can cause significant, even life threatening, problems.
Risk factors
The commonest risk factors are acquired and include cigarette smoking, age (> 40 years of age), hypertension (high blood pressure) and recreational drug abuse (cocaine or amphetamine).
Although these risk factors increase a person's risk, they do not necessarily cause aneurysm formation or rupture. Some people with one or more risk factors never develop the disease, while others develop aneurysms and have no known risk factors. Knowing your risk factors to any disease can help to guide you into the appropriate actions, including changing behaviours or seeking medical advice.
Presentation Of Aneurysms
The first evidence of a cerebral aneurysm may be a subarachnoid haemorrhage (SAH), due to rupture of the aneurysm. This can present as the “worst headache in my life", neck stiffness, nausea and vomiting, loss of consciousness and photophobia (sensitivity to light).
If any of these symptoms occur they signify a medical emergency and help should be sought immediately from your GP or local hospital.
Often cerebral aneurysms are identified as incidental findings in various scans of the head, usually for unrelated conditions. These are unruptured aneurysms and they are usually not an emergency, although they require expert assessment and management.
Such patients are usually seen by a neurosurgeon, ideally with a special interest in brain aneurysms and subsequent management of these unruptured lesions is delivered by team of experts in neurosurgery, neuroradiology and neurology (neurovascular multidisciplinary team).
Treatment of Aneurysms
Treatment of these lesions depends if they have ruptured or not. Ruptured aneurysms (SAH) are a medical emergency and immediate hospital admission and review by a consultant neurosurgeon is warranted. A CT scan of the head is diagnostic in 99% of the cases, although some patients may require further tests like a lumbar puncture to confirm that a rupture has occurred.
Early treatment is aimed at supporting the patient and securing the aneurysm to protect from repeat bleeds.
Treatment can be either through the arteries/veins (endovascular coiling) or through an open operation (craniotomy). The decision on the best mode of treatment is taken after special investigations have been performed and the patient reviewed by a neurosurgeon with a special interest in the treatment of aneurysms.
Arteriovenous Malformations (AVMs)
Normally blood flows from the heart to the arteries of the body. The arteries branch and get smaller until they become a capillary, which is just a single cell thick. In this way blood pressure drops to very low levels that the thinner walled veins can cope with. In an arteriovenous malformation (AVM), usually early in life, arteries connect directly to veins. This is a high-pressure shunt or fistula. Veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge and create what we call a “nidus”. Usually there are multiple feeding vessels in an AVM and many draining veins.
Symptoms of Arteriovenous Malformations
The symptoms of AVMs vary depending on their type and location. While migraine-like headaches and seizures are general symptoms, most AVMs do not show symptoms until a bleed occurs. Common signs of brain AVMs include the sudden onset of a severe headache, vomiting, a stiff neck, seizures, migraine-like headaches or a Bruit.
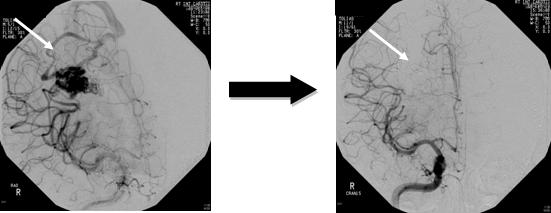
Treatment of Arteriovenous Malformations
Surgery, endovascular therapy, and radiosurgery can be used alone or in combination to treat an AVM. Endovascular embolization is often performed before surgery to reduce the AVM size and risk of operative bleeding. Radiosurgery or embolization may be used after surgery to treat any remaining portions of the AVM. Your neurosurgeon will discuss with you all the options and recommend a treatment that is best for your individual case.
Observation
If there have been no previous hemorrhages, the doctor may decide to observe the patient, which may include using anti-convulsants to prevent seizures and medication to lower blood pressure.
Radiosurgery
Radiosurgery aims a precisely focused beam of radiation at the abnormal vessels. The procedure takes several hours of preparation and one hour to deliver the radiation. The patient goes home the same day. After six months to two years, the vessels gradually close off and are replaced by scar tissue. The advantage of this treatment is no incision and the procedure is painless. The disadvantages are that it works best with smaller AVMs and may take a long time to show effect (during which time risk of hemorrhage exists).
Endovascular therapy
Endovascular treatment uses small catheters inserted into your blood vessels to deliver glue or other obstructive materials into the AVM so that blood no longer flows through the malformation. It is performed in the angiography suites of the Radiology Department by a neurointerventionalist. The procedure is performed under general anesthesia. A small incision is made in the groin and a catheter is inserted into an artery then passed through the blood vessels to the feeding arteries of the AVM. Occluding material, either coil or acrylic glue, is passed through the catheter into the AVM. The procedure time can vary, and the patient remains in the hospital several days for observation. The advantage of this treatment is that it is less invasive than surgery and can be used to treat deep or inoperable AVMs. Disadvantages include the risk of embolic stroke from the catheter and re-bleeding since the AVM is not completely obliterated. Multiple treatments may be necessary.
Surgery
Using general anesthesia, a surgical opening is made in the skull, called a craniotomy. The brain is gently retracted so that the AVM may be located. Using a variety of techniques such as laser and electrocautery, the AVM is shrunk and dissected from normal brain tissue. The length of stay in the hospital varies between five to seven days with some short-term rehabilitation. The type of craniotomy performed depends on the size and location of the AVM. The option of surgery also depends on the general health of the patient. The advantage of surgical treatment is that a cure is immediate if all the AVM is removed. Disadvantages include risk of bleeding, damage to nearby brain tissue, and stroke to other areas of the brain once removed.
For further information on the author of this article, Consultant Neurosurgeon, Mr Ranjeev Bhangoo, please click here.
An AVM or arteriovenous malformation forms when arteries connect directly to veins. This direct connection forms a high-pressure shunt or fistula. The veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge to create a “nidus”. Usually there are multiple feeding vessels in an AVM and many draining veins.
Full medical glossaryAn AVM or arteriovenous malformation forms when arteries connect directly to veins. This direct connection forms a high-pressure shunt or fistula. The veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge to create a “nidus”. Usually there are multiple feeding vessels in an AVM and many draining veins.
Full medical glossaryAssociated with the nervous system and the brain.
Full medical glossary


