This article takes an informative look at pain medicine, what they are used to treat and the different types of pain and painkillers. This article will be of interest to anyone who is suffering from nociceptive or neuropathic pain and would like to know what their treatment options are.
Contents
- Understanding different types of pain
- The analgesic ladder
- Neuropathic pain
- What is the ideal pain killer?
We can take a sample of blood from a patient and measure the levels of hundreds of substances in it; we can use x-rays, ultrasound, MRI, and radioisotopes to image any part of the body in minute detail. We can even take a sample of hair and tell if someone had taken drugs months previously. But if a patient tells us they’re in pain we can’t measure their pain in a blood sample, or look at it on an x-ray, and we certainly can’t tell from their hair that they were in pain a few months earlier. We have to believe them, and a good doctor will always believe their patients if they tell them they’re in pain. Pain is entirely subjective.
We may not be able to visualise pain or to measure it objectively but we can ask patients to rate their pain by comparing it with other painful experiences they have had in their lives. In clinical practice this is what we do most often. We typically ask them to mark their pain on a 10 cm line or to tell us from 0 to 10 how bad their pain is, where 0 is no pain at all, and 10 is the worst pain they can possibly imagine.
Understanding different types of pain
Very importantly though, there are different types of pain, and it is important to establish the type of pain a patient is experiencing as different types of pain require completely different treatments. The type of pain we are all used to and which we all understand is called “nociceptive.” This is the sort of pain we experience when we break a bone, cut ourselves, or have an operation. The other main type of pain is caused by damaged or malfunctioning nerves. This is called “neuropathic” pain. Neuropathic pain is very different from nociceptive pain. Patients generally find it far more painful that nociceptive pain, and it does not respond well at all to normal painkillers.
The analgesic ladder
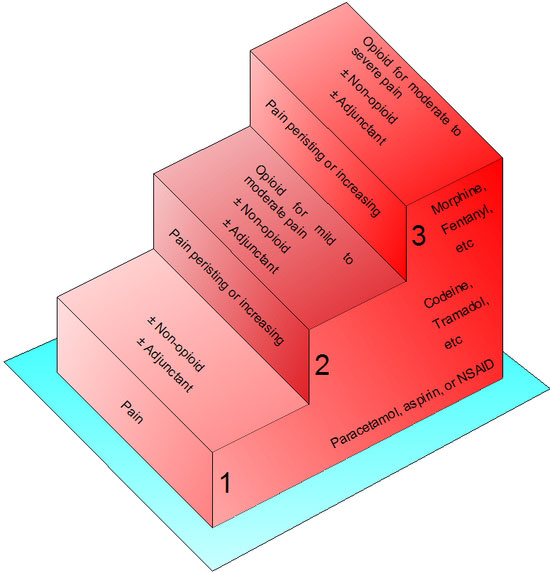
When we are prescribing painkillers for nociceptive pain we use what is called an analgesic ladder. This was developed by the World Health Organisation for managing patients with pain from cancer. At the lowest level are simple analgesics such as Paracetamol and Ibuprofen or other non-steroidal anti-inflammatory drugs (NSAIDs). The NSAIDs are very useful for bone and joint pain and are often used as a first line medication for patients with arthritis or other age-related skeletal problems. Paracetamol has been shown in some studies to be as effective as morphine in certain situations and it is an under-rated drug. It is important to take analgesics regularly during the day, and not to take them only if the pain gets really bad. If simple analgesics aren’t strong enough we go up to the next step where there are mild opioid drugs such as Codeine, drugs with mixed opioid and non-opioid effect such as Tramadol. At this step mild opioids are often combined with simple analgesics. Examples at this level include Co-Codamol (Paracetamol + Codeine) and Co-Dydramol (Paracetamol + Dihydrocodeine).
The final step is strong opioids. There are many drugs as this level; the best known drug and still the most widely used is Morphine, but there are also many other drugs such as Diamorphine (better known as heroin), Pethidine, Oxycodone, Hydromorphone, Buprenorphine, and Fentanyl. They all differ slightly in such features as their effects and routes of administration. Morphine is the mainstay of opioids for use in patients in severe pain whether from cancer or after surgery, but the subtle differences between these drugs can be crucially important to the patients who need them. For example Oxycodone can be helpful for patients who have some component of neuropathic pain; Fentanyl and Buprenorphine can be absorbed through the skin and are available as self-adhesive patches that are changed every few days; Fentanyl is also available as a lozenge that can be put under the tongue, which can be very useful for patients who cannot swallow. There were photographs of Jade Goody in her final few weeks with a Fentanyl lozenge in her mouth.
Opioids can be very effective at relieving pain but this comes at a price. They cause constipation at relatively low doses, and patients can quickly become very uncomfortable. They can also cause nausea and sickness, suppress patients’ appetites, and cause depression of breathing. This last side-effect is the commonest cause of death in inadvertent overdose, or if heroin addicts take an overdose. The side effects can normally be managed by paying careful attention to detail, such as by prescribing laxatives and anti-emetics.
Neuropathic pain
We haven’t yet talked about neuropathic pain. It is a very different creature altogether. It can be managed in a lot of cases by conventional “anti-nociceptive” analgesics, but these often have to be given in enormous doses. Patients often use words such as “burning”, “gnawing”, “electric shock,” or “shooting” to describe it. Many describe it as being like constant toothache. It can occur anywhere in the body, from the scalp and face to the toes. It is often accompanied by altered sensations in the skin. The commonest of these is something we call “allodynia”, which is an intense burning pain that can last for up to an hour after even light touch, wind blowing on the skin, or even if clothing touches the area. The skin pain and sensitivity of allodynia only happen to people who have neuropathic pain - nothing else causes it.
Neuropathic pain has to be treated with a special group of drugs – drugs that modify nerve function, rather than drugs that act at the site of injury or in the brain. These include drugs such as Amitriptyline or Nortriptyline, which used to be used in much large doses as antidepressants. There are also drugs such as Gabapentin and the newest drug Pregabalin, which are increasingly being used as first line medication for the treatment of neuropathic pain.
For small patches of skin with neuropathic pain we can use local anaesthetic patches impregnated with the local anaesthetic drug Lidocaine, or a drug called Capsaicin, which is derived from chilli peppers and contains a substance which depletes the pain chemicals from nerve endings in the skin.
What is the ideal painkiller?
We need strong analgesics with fewer side effects and longer durations of action. We also need more effective anti-neuropathic drugs, and better local anaesthetic drugs with better ways to administer them, but on the whole we can manage pain much better now than we have been able to in the past. We are making incremental improvements year on year and we now usually combine together a number of different pain medications with slightly different modes of action. And wherever possible if there is a clearly localised problem we can do a wide range of image guided procedures such as destroying tumours, treating painful joints, or knocking out nerves that carry pain signals to the brain. We can satisfactorily control pain and other symptoms in nearly all patients in pain.
For further information on the author of this article, Consultant Interventionalist Spine and Pain Physician, Dr Nigel Kellow, please click here.
Non-steroidal anti-inflammatory drugs. A group of drugs that provide pain relief and reduce inflammation.
Full medical glossary








