Why should you take varicose veins seriously?
Varicose veins are veins that have become enlarged swollen and twisted. Although any vein can become varicosed it is the veins in the legs that are usually affected. Varicose veins are often considered to be simply a cosmetic issue but this misconception is not altogether true. It is very important to understand that vein disease can go beyond the appearance of varicosities and could progress to complications such as skin damage, ulceration, blood clots (thrombosis) and in the worse case scenario a blockage in the lungs (pulmonary embolism), which can be fatal. An early assessment and appropriate intervention can help mitigate against these risks.
It is perhaps surprising to note that vein disease represents two per cent of the total healthcare budget of the UK, with most of this cost being attributed to the treatment of venous leg ulcers. It is estimated that seventy-three thousand people in the UK suffer from this condition. The appearance of veins on our legs should therefore be taken seriously.
Why do varicose veins form?
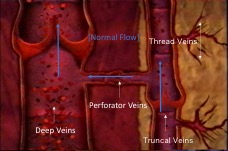
Unlike arteries, which take oxygenated blood from the heart, veins allow blood to drain back, primarily with the help of our calf muscles and supported by valves which prevent blood draining backwards under the effect of gravity. In a healthy vein, blood drains from the truncal veins through to the deep vein system via perforators. (see opposite)
As well as the veins we can see just under our skin, there are also slightly deeper veins that arise from the groin. These are called the great saphenous vein (GSV), accessory anterior thigh vein (AATV) and small saphenous vein (SSV).
Blocked truncal veins

The relationship between these larger truncal veins and the smaller veins can be thought of as similar to rivers and tributaries. Water flows from the tributaries into the rivers and out to sea. If there is a blockage or obstruction to the flow of water in the river the tributaries build up with water, bulge and eventually burst their banks. Our veins work in a very similar way, a blockage (eg from DVT) or leaky valves in the larger truncal veins causes a build-up of pressure in the numerous smaller veins connected to them. As the pressure builds, the veins bulge and become visible on the surface of the skin. In extreme circumstances these veins can bleed (haemorrhage), or cause severe skin discoloration and swelling - and in some cases lead to leg ulcers.
Therefore, by treating the GSV or SSV, the pressure is taken off the smaller visible veins, stopping the back pressure from the malfunctioning veins. Treatment of truncal veins depressurises the whole system, much like deflating a balloon.
 You might ask, if treatment effectively destroys these truncal veins, how does the blood get back to the heart? The fact is that 90% plus of our blood is drained back to the heart in the deep vein system, meaning that the smaller veins play a very small part. The body adapts to losing these veins and the overall function of the circulatory system improves.
You might ask, if treatment effectively destroys these truncal veins, how does the blood get back to the heart? The fact is that 90% plus of our blood is drained back to the heart in the deep vein system, meaning that the smaller veins play a very small part. The body adapts to losing these veins and the overall function of the circulatory system improves.
What causes varicose veins?
The main theory is that the valves in the truncal veins start to fail, often with age. Instead of heading back up to the heart, blood returns down the leg towards the foot. This is called reflux and it is this that ultimately causes the pressure to build and for varicose veins to form.
Blood reflux and valve failure
Valve failure can be seen as a chain reaction. A failing valve higher up the leg, creates greater pressure on the valve below. This causes further vein distention and, in turn, further valve failure lower down.
This build-up of pressure above the valve can lead to secondary valvular incompetence. As the vein wall dilates the vein becomes larger and wider, it stretches the valves apart causing them to fail. It is referred to as 'secondary' because the valve failing isn’t the primary reason for the reflux. The primary cause is likely to be the result of a genetic weakness in the vein wall. Most people don’t have valves above the groin so reflux problems are generally an issue of the lower leg.
Perforator valve failure - no rush to treat
When perforator valves fail, you would think there would be backwards pressure from the deep vein system, but this isn’t always the case. This is a major reason why surgeons shouldn’t rush to treat perforator valves. If the deep veins are working fine then they will release pressure in the system. Perforator valve failure is often a secondary issue which is why we don’t spend time trying to fix them. Failure of these valves does not impact the superficial system (GSV, SSV) because the deep veins are working fine.
Types of varicosity
1. Truncal 
Big bulgy veins on the back of the calf or side of the leg. These main veins run along the outside of the muscle but under the skin. They would not normally be visible as they lie inside the layer of fat just under the skin, although in very slim people sections can be seen on the surface. Virtually all visible vein problems on the surface stem from at least one of these truncal veins. These veins include:
- Great Saphenous Vein (GSV)
- Small Saphenous Vein (SSV)
- Anterior Accesory Saphenous Vein (AASV)
- Giacomini Vein (GV)
2. Reticular & Telangectasia 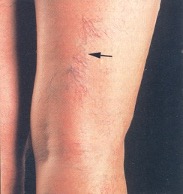
Smaller ‘spider’ or ‘thread’ like veins on the surface of the skin
Veins that appear reddish / blue in colour can often be seen through the skin, especially around the joints. When they bulge, they may have become varicose, however if visible and flat, they are just called reticular veins. If there are coloured, tiny veins on the surface they are called thread veins. Reticular veins may be normal and a diagnosis is needed to tell using duplex ultrasound. However, thread veins are always abnormal.
3. Malformations 
Although sometimes referred they are not actually varicose veins. These are abnormal veins and extremely uncommon. Where you can see them, they are easily treated with foam sclerotherapy under local anaesthetic.
Don’t wait, get treatment early to avoid nasty complications
What is the nature of varicose veins?
Varicose veins are primarily caused by genetic weaknesses, but the disease is exacerbated by lifestyle factors. If your parents had them, then the chances are you will have them too. There isn’t a lot you can do to prevent it, but don’t wait, get treatment early to avoid nasty complications. In all probability vein disease will only get worse. With pregnancy, 80% of women will normally develop varicose veins. This again is related to the additional pressure burden on the circulatory system and in most cases, these will disappear after childbirth.
Vein disease is also linked to obesity and this is likely to be related to the additional pressure on the valves due to higher blood pressure.
When should I seek treatment?
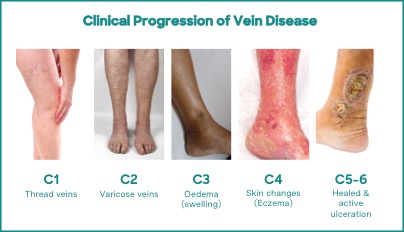 Varicose veins are rated clinically according to a comprehensive classification system for chronic venous disease, or CEAP scale, which ranges from C1 to C6, with C6 being the most severe.
Varicose veins are rated clinically according to a comprehensive classification system for chronic venous disease, or CEAP scale, which ranges from C1 to C6, with C6 being the most severe.
The illustration (right) shows a typical visual representation of the scale.
Unfortunately for sufferers of varicose veins, there is no reliable way of predicting whether they will progress onto more serious complications. If you take one hundred patients with varicose veins, you know that around ten will go on to develop a leg ulcer, however you just don’t know which ten.
This is why the latest guidance recommends a detailed duplex scan as soon as evidence of vein disease becomes visually apparent, whether for small thread veins or the larger truncal varicosities. This scan evaluates the health of the deep vein system. There is currently no evidence at all to say that the size of a varicose vein determines the propensity for further complication.
What complications can develop with varicose veins
The main complications of varicose veins relate to the progression of vein disease, and these include:
- haemorrhage,
- thrombophlebitis,
- skin changes (discoloration and eczema), and
- leg ulcers
Haemorrhage caused by vein disease
Bleeding occurs when the superficial covering of skin over a varicosity breaks. This is not necessarily painful; many people aren’t even aware of bleeding until they see large quantities of blood that had previously been pooled within the vein. Usually, it is the dark blue and black veins covering the legs that break the skin. Often, it’s just a trivial bump or minor injury that leads to a bleed and whilst not always the case, this can go on to become a leg ulcer.
Thrombophlebitis caused by vein disease
 This is where small blood clots form in the veins and they become hard and inflamed. This uncontrolled hardening of the blood in the vein can be very painful. This condition unfortunately often gets misdiagnosed as an infection and patients wrongly get prescribed antibiotics. The latest European Society of Vascular Surgery guidelines recommend treating patients initially with anti-coagulation drugs. Once the veins have settled down, they should then be treated to stop it reoccurring and specifically because of the increased risk of deep vein thrombosis (DVT). Overall, there is a reasonable risk (around 5%) that you’ll go on to get DVT if you get superficial vein thrombophlebitis.
This is where small blood clots form in the veins and they become hard and inflamed. This uncontrolled hardening of the blood in the vein can be very painful. This condition unfortunately often gets misdiagnosed as an infection and patients wrongly get prescribed antibiotics. The latest European Society of Vascular Surgery guidelines recommend treating patients initially with anti-coagulation drugs. Once the veins have settled down, they should then be treated to stop it reoccurring and specifically because of the increased risk of deep vein thrombosis (DVT). Overall, there is a reasonable risk (around 5%) that you’ll go on to get DVT if you get superficial vein thrombophlebitis.
Skin discoloration and eczema caused by vein disease
Discoloration is caused by blood leaking into the tissue surrounding the vein. When this blood gets naturally reabsorbed, it leaves behind the iron component of the blood. This process is called hemosiderin and leaves brown stains on the skin, literally like rust!
 Some people think it’s a sun tan or don’t notice it. The residual material causes irritation which can also progress to eczema.
Some people think it’s a sun tan or don’t notice it. The residual material causes irritation which can also progress to eczema.
The process starts with a hardening of the fat in the skin with brown discoloration, known as lipodermatosclerosis. The skin loses elasticity and becomes prone to breaking down and becoming damaged. Once damaged, an ulcer can be triggered, either spontaneously or as a result of accidental injury.
Skin changes including brown stains on the thigh, with little flare veins on the surface are known as corona phlebectatica. These have been upgraded in the latest guidance to C4. They’re a clear sign of advanced disease progression where skin changes in the ankle are directly associated with flare veins in the thigh.
Venous leg ulcers caused by vein disease
If you have a leg ulcer you should treat the veins as early as possible
A venous leg ulcer is an open wound in the leg where vein disease is the primary underlying cause. Over 70% of patients with venous ulcers also have varicose veins. Overall, its estimated that over seven hundred and thirty thousand people in the UK suffer from these ulcers. Given the current guidelines on funding varicose veins, these often get referred to nurses to dress the superficial wound, rather than a vascular specialist to treat the underlying cause. However, there is now good evidence from a number of different studies, showing that if you have a leg ulcer you should treat the veins as early as possible because it helps with their healing.
It used to be thought that you should only treat the varicose veins once the ulcer has healed but this is not correct. Treating the veins early enhances healing and reduces recurrence.
Conclusion
In conclusion, then, it is very important to be aware that varicose veins are a tangible sign of vein disease. They can be the precursor to serious complications and should not be ignored.








