This article, written by an expert in breast cancer and breast surgery, outlines the advances in reconstruction following breast cancer surgery and includes information on the different types of implants and surgical techniques.
Contents
- Introduction
- Breast implants
- Breast reconstruction
- Role of mesh
- Examples of standard skin-sparing mastectomy (SSM)
- Nipple reconstruction
- Nipple preservation
Introduction
Approximately one in five patients with breast cancer will require a mastectomy rather than a lumpectomy. As mastectomy results in the distortion of the body image, it is natural for some patients to seek reconstructive surgery. However, some women just want to have the cancer removed and are not keen on having breast reconstruction. Although an external implant is available that is worn inside the bra this is inadequate for many women.
The choice of reconstruction surgery depends upon a woman's build, shape and size of her breasts, previous scars, and her own preferences.
Breast implants
An implant is inserted under a muscle in the chest wall at the mastectomy site. Implant reconstruction can be performed immediately at the time of skin-sparing mastectomy or as a delayed procedure through the original mastectomy scar. There has been a recent concern regarding the safety of silicone implants. In fact, there is no evidence that FDA-approved silicone implants (Allergan and Mentor brands) increase the incidence of breast cancer or other diseases, such as arthritis. The main problems with implants are infection (occurring in 2% of patients) and scarring around the implant. Scarring makes the breast feel hard and painful, which is more common if the prosthesis is very smooth.

![]()
Modern implants consist of an outer silicone shell (roughened or textured) and an inner compartment that can be filled with saline (salt water) instead of silicone gel. Implants having a similar shape to the natural breast have recently been introduced. Your breast surgeon will explain the pros and cons of the various types of implant available to you and you should request to see pictures showing the outcome of the various methods.
Breast reconstruction
All patients undergoing mastectomy should be offered the possibility of breast reconstruction, either performed immediately at the time of the mastectomy, or as a later procedure. Mastectomy combined with immediate reconstruction is preferred and seems to cost less than mastectomy with subsequent delayed reconstruction. There is no evidence that immediate reconstruction at the time of mastectomy worsens the breast cancer outlook. Frail patients with other medical problems are not advised to undergo breast reconstruction surgery as they have a higher risk of complications.
There are various methods of reconstruction and the choice should be made after discussion with the breast surgeon, specialist breast nurse and other patients who have had breast reconstruction. I prefer the type of mastectomy that preserves most of the natural skin envelope of the breast (called a skin-sparing mastectomy) when performing immediate breast reconstruction due to the superior cosmetic result.
Role of mesh
Conventionally, the use of under the muscle implants has been restricted as expansion of the lower pole (infra-mammary fold) involves repeated sessions of gradual inflation of the implant to achieve a natural profile. The acellular tissue matrix has been shown to incorporate well into human tissues, with no rejection. The most commonly used tissue matrix (Strattice®) is derived from porcine (pig's) skin and does not contain any cellular DNA. This matrix allows for one stage breast reconstruction using a fixed-volume silicone implant and has widened the scope of implant-based breast reconstruction. Incorporation of the mesh results in an intact acellular matrix of natural biological components that promote rapid re-vascularisation and cell re-population around the implant thus improving the cosmetic result and feel of the implant.
Examples of standard skin-sparing mastectomy (SSM)
The skin-sparing mastectomy method of reconstruction involves the removal of the latissimus dorsi flap from the back for use in the reconstruction. For further information please click here.
Other methods of reconstruction include breast implants, either saline-filled tissue expanders or silicone implants.
Surgery carried out by the author, Kefah Mokbel, in 2003 (viewable on the link below) shows the long-term cosmetic result of SSM plus latissimus dorsi flap reconstruction. A 52 year old lady had right skin-saving mastectomy and immediate breast reconstruction using a skin and muscle flap from the back for early breast cancer. She also had nipple reconstruction and enlargement of the opposite breast in order to achieve symmetry.
NB: To view this surgery please click here. This image must only be viewed by persons over 18 years of age.
The following image link shows a left skin-saving mastectomy and immediate breast reconstruction using a skin and muscle flap from the back for early breast cancer in a 49 year old lady. She also had nipple reconstruction and tattooing.
NB: To view this surgery please click here. This image must only be viewed by persons over 18 years of age.
The image found on the link below shows the long-term result of an immediate breast reconstruction in a 47 year old woman. She had a bilateral SSM using implants followed by radiotherapy to the right breast and nipple reconstruction using small local flaps and tattooing.
NB: To view this surgery please click here. This image must only be viewed by persons over 18 years of age.
Nipple reconstruction
It is also possible to reconstruct the nipple using local skin, a portion form the opposite nipple, or a skin graft taken from the groin. The new nipple can be tattooed to make it a similar colour to that of the opposite nipple. A disposable tattooing instrument is used to minimise the risk of disease transmission.
The following image link shows the post-surgery result of a nipple reconstruction prior to tattooing.
NB: To view this surgery please click here. This image must only be viewed by persons over 18 years of age.
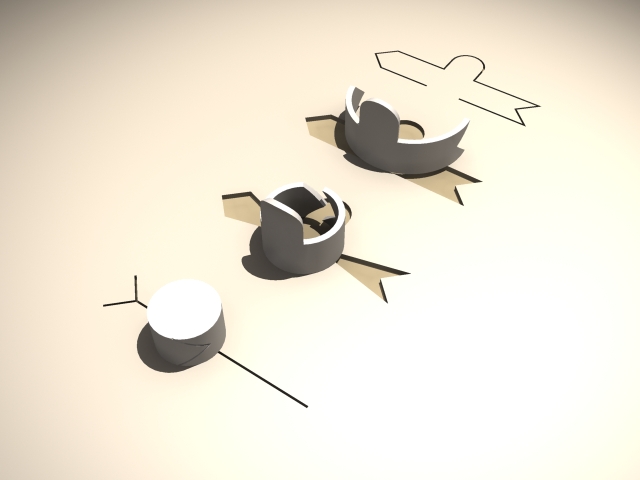
From top right to bottom left this figure shows the steps of performing a nipple reconstruction using a small local flap.
Nipple preservation
In selected cases the nipple can be preserved during skin-sparing mastectomy and reconstruction in order to achieve a superior cosmetic result.
The photo found on the link below shows the excellent cosmetic result from bilateral nipple-saving mastectomy and implant reconstruction in a 40 year old diagnosed with breast cancer.
NB: To view this surgery please click here. This image must only be viewed by persons over 18 years of age.
For further information please see the following article by Prof Kefah Mokbel and colleagues.
Reefy S, Patani N, Anderson A, Burgoyne G, Osman H, Mokbel K. 2010. Oncological outcome and patient satisfaction with skin-sparing mastectomy and immediate breast reconstruction: a prospective observational study. BMC Cancer 10:171.









