Up to ten per cent of women who have had breast surgery go on to suffer chronic pain for up to twelve months following surgery. Early pain control is therefore critical.
Contents:
- Pain Management following Breast Surgery
- Use of Surgical Drains following Breast Surgery
- Type of Paun Relief Needed following Breast Surgery
- Achieving Best Outcomes following Surgery for Breast Cancer
- Post- breast cancer surgery drain management
- Pre-operative pain relief
- Intra-operative Pain Relief
- Post-operative Pain Relief
Pain Management following Breast Surgery
Breast cancer is of course a serious disease that sometimes can only be treated surgically with a mastectomy. A percentage of women undergoing surgery also opt to have reconstruction performed at the same time. The postoperative management and care for these women greatly affects both the cosmetic and psychological outcome of the surgery and is in my view absolutely fundamental.
A recent study carried out by the Helsinki University Central Hospital in Finland of more than 800 women who had undergone surgery for breast cancer has shown that many were still suffering some level of pain 12 months after their surgery. However, this regrettably did not come as a surprise as the National Mastectomy and Breast Reconstruction Audit (revised October 2012) had revealed similar findings. This was one of the most important audits in recent times to look at the outcomes of surgery and particularly at what is known as patient reported outcomes, or PROMS. These were gathered by patients completing questionnaires at 3 and 18 months following surgery and the data collected provided new and important insights into the patient experience following breast cancer surgery.

Within these outcomes it was found that 8% of patients remained in pain most or all of the time after immediate reconstruction and 9% after delayed breast reconstruction. Although these numbers may be relatively small in percentage terms, chronic pain has a devastating effect on the lives of the women that they represent and improving early pain control could have a big impact on the long term outcomes of surgery.
In direct response to the findings of the audit I have been working closely over the last two years to analyse the pain control methods in own my practice and to develop and refine pre-operative, peri-operative and post-operative pain management strategies, so as to improve outcomes for my patients.
Traditionally there was no formal pathway in place for post-operative pain relief for breast patients and I therefore began by carrying out an audit of an array of available painkillers. Then, following the experience of a single surgeon / single anaesthetist approach in complex breast surgery patients with good pain outcomes, I have adopted a standardised approach to best manage pain in breast surgery patients in my practice.
The use of surgical drains following breast surgery
When examining the issue of pain following breast surgery it is crucial to consider how vacuum drains are used. Vacuum drains are inserted into the breast after surgery to allow blood and tissue fluid to be removed from the wound. This initially aids wound healing and helps to prevent the fluid that seeps out from small blood and lymphatic vessels damaged during the surgery from collecting under the wound (called a seroma.) Vacuum drains also allow the surgical team to be aware of any problems with wound bleeding, which sometimes can requires a short further operative procedure.
The drain comes out through the skin and it is this site that is often a source of significant pain and local tenderness. In addition, leaving drains in for too long presents a risk of infection and the suction of the vacuum can actually increase wound fluid output, delaying both the healing process and discharge from hospital.
The policy in my hospital was for a patient to have a drain removed if the fluid output was less than 100ml in 24 hours. This leads to inpatient stays of two to three days on average with some patients staying for up to five days. When we audited this policy it was found to have little impact on fluid collection under the skin and probably actually increased the infection risk. As the process was leading to patients having to stay in hospital for longer with little benefit we revised it.
Type of pain relief needed following breast cancer surgery
The principle that underlies the type of pain relief that I now use in my breast cancer surgical practice is based on utilising several approaches to pain control directed at many different pain pathways and receptors, starting at the induction of anaesthetic and continuing during the surgery and into the post-operative period. By addressing the pain pathway early on patients wake up in little pain and this in turn reduces levels of anxiety and further pain and prevents a cycle of ongoing pain from occurring. By using several types of analgesic drugs different pain receptors can be targeted simultaneously. In addition, the use of large volumes of lower concentration local anaesthetic allows more effective infiltration of the surgical site and gives a more effective level of local pain control, for example, at the site of the surgical drains. This use of local anaesthetic means that patients wake up free of pain and by the time that it wears off they are able to eat and drink and take regular simple painkillers such as paracetamol and ibuprofen.
Achieving the best outcomes following surgery for breast cancer

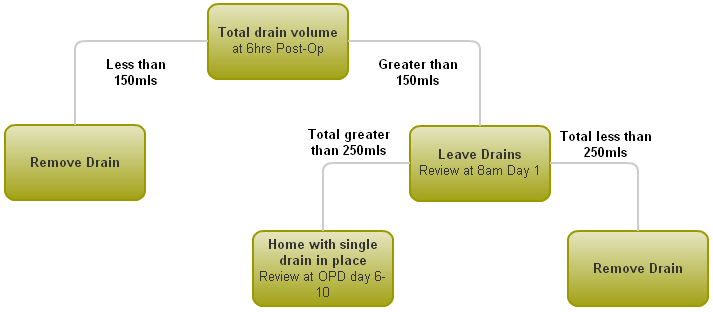
Following the outcome of the audits that I carried out both into pain management and the use of drains following surgery for breast cancer I have now put into effect new protocols that I believe offer the best post-surgery outcomes for patients. Two vacuum drains are inserted during the surgery and the contents of these drains are measured at 6 hours post operation. If the fluid volume is less than 150mls in total they can be removed at that time. If it is greater than 150mls the drains will remain in place and they will be reviewed at 8am on day 1 post-operation. If the total fluid volume at that point is less than 250mls then the drains are removed and the patient can be discharged. If the fluid volume is more than 250mls the patient can be discharged with a single drain in place that will be removed during clinic on day 6 to 10 following surgery. If a patient requires a change of drain bottle then they can telephone the ward directly to arrange to attend for this to happen.
For patients undergoing a latissimus dorsi (LD) tissue-flap based reconstruction using muscle taken from the back the drain management will be individualised rather than protocol driven.
Pathway for post-surgery drain management (all cases excluding LD flap reconstruction)
In addition, I have put in place the following pain relief plan for all my breast surgery patients:
Pre-operative pain relief
I make sure that each patient has a standardised prescription of simple pain control and anti-sickness medication.to ensure timely and regular administration following the surgery. This avoids the all too common situation of a patient in pain asking for pain relief, waiting until it is prescribed and then receiving it well after the onset of the pain itself.
Intra-operative pain relief
I use sophisticated monitoring to titrate the levels of intravenous pain control drugs to the meet the patient’s needs. This removes the requirement for a "slug" of morphine that can result in many patients waking up with nausea and vomiting following the anaesthetic. In addition, direct infiltration of local anaesthetic during the operation itself into the nerves supplying for example chest wall sensation, allows accurate local anaesthetic cover and good regional pain control. By infiltrating the nerves themselves rather than just the skin where the incision is, better pain control can be achieved.

Post-operative pain relief
Injections of blood thinning medicines ensure that deep vein thrombosis is prevented. My patients are encouraged to eat and drink and to get up immediately. The removal of drains as soon as possible (usually after 6 hours if no bleeding has occurred), allows patients to become mobile quickly and avoids drain sites becoming sore and tender and patients being stuck attached to many tubes and drips.
Conclusion
Considerable advances have been made in the surgical techniques for treating breast cancer over recent years and these have led to greatly improved outcomes for patients. However, it is very easy to overlook the fundamental impact that persistent and prolonged pain can have on the quality of life for women who have undergone surgery for breast cancer when focussing solely on survival statistics and success rates. It is therefore important that every effort is made to ensure that women are not let down in this way.








