This article discusses a new and innovative technique to reverse the deterioration of the joints. We believe that the information here will be of help to anyone who suffers from osteoarthritis or joint pain and would like insight into new non-invasive treatments when other treatments may have failed.
This will seek to answer 'what is knee osteoarthritis?', 'what knee treatments work?' and 'are there alternatives to knee surgery?'.
Contents - The Biomechanics of Knee Pain
- Introduction to the biomechanics of knee pain
- Methods of adjusting the knee joint
- Rehabilitating gait
- Knee biomechanics
- Current biomechanical therapies for knees
- AposTherapy
- Centre of pressure – it starts at ground level
- Controlling pressure through feet, ankles, legs, pelvis and spine
- Conclusion
Introduction
This article aims to provide an understanding of the biomechanics involved in the knee and explains how a non-invasive biomechanical adjustment of the joint may be a better option than surgery.
Growing evidence points to the importance of biomechanical factors on knee osteoarthritis. The key feature of knee osteoarthritis is that it is characterised by decreased neuromuscular control, instability of the knee joint and weakness of the knee muscles, all of which leads to an abnormal bracing of the knee. This abnormal bracing causes the knee to move differently and this change from the more normal movement can be measured by specialists. A problem occurs when the weight of the body is localised on just one part of the joint – known as the posterior medial aspect of the knee. The increase in knee joint loading causes further deterioration of the joint cartilage and worsens the symptoms of osteoarthritis. The changes place the patient in a vicious cycle with further deterioration of clinical symptoms, such as pain and dis-function.
Methods of adjusting the knee joint
There have been many attempts to try to stop and even reverse this cycle. Most of them focus on redistributing loads on the affected joint and returning the musculoskeletal properties of the knee back to the normal healthy pattern. Examples include orthotics, braces and walking aids. Physical exercises and neuromuscular training, such as training with unstable surfaces, are also being examined. All these interventions, however, have had limited success from a clinical point of view and have yet to show evidence of stopping/changing the biomechanical deterioration of the knee.
However, more recent studies have examined a new biomechanical therapy for the management of knee osteoarthritis called AposTherapy. This treatment has shown that patients with knee osteoarthritis who were treated with AposTherapy reported a significant reduction in pain and an improvement in function, quality of life and gait patterns. In some instances there has actually been a reversal of the biomechanical abnormalities.
Rehabilitating gait
This new approach rehabilitates the damage causing gait patterns of patients with knee osteoarthritis. The therapy is based on a unique technology that enables manipulation of the centre of pressure under the foot, which modifies the moments acting on the joints of the lower limb, pelvis and spine. Throughout this therapy the patients are carefully monitored for changes in gait, pain and function.
Knee biomechanics
Biomechanical factors such as abnormal posture and mal-alignment of the joints lead to greater loads on the affected joint. Other factors, such as muscle weakness and neuromuscular deficits, lead to compensatory mechanisms such as co-contraction and bracing that further harm the joint. The associated pain arises in response to increased loads on the affected joint. High levels of pain lead to exercise avoidance and, when severe, even an avoidance of daily life activity such as walking and climbing stairs.
Treating the biomechanical factors of knee OA
Due to the well-established evidence of the effect of biomechanical factors on knee osteoarthritis, there is a growing experimental and developmental effort to find an adequate biomechanical intervention for knee osteoarthritis. The overall goal is to find a solution that will stop the deterioration of the disease and hopefully even reverse its pathogenesis. Current research focuses on finding biomechanical methods that reduce loads from the affected joint and rehabilitate muscle activity. Clinicians have attempted to reduce knee joint loads through biomechanical devices such as orthotics and knee braces. These interventions aim at reducing the knee adduction moment. The principle for muscle rehabilitation is based on training and improving neuromuscular control. To date, biomechanical therapies have had limited clinical success and have yet to show evidence of reversing the abnormal biomechanical patterns of knee osteoarthritis. Furthermore, none of the therapies integrate both load reduction and muscle rehabilitation.
Current biomechanical therapies for knees
Knee braces, orthotics, walking aids and similar intervention are the usual therapies in use today. Exercises on unstable surfaces are also being examined as therapies for improving neuromuscular control. These therapies have all had limited clinical success and not shown evidence of reversing the abnormal biomechanical patterns of knee osteoarthritis.
Neuromuscular exercises on unstable surfaces are limited to date and mostly include exercises on a stationary wobble board. Such exercises do not allow for control of the biomechanical alignment in the knee and as such may cause pain during exercise. Exercising while in pain affects proper motor learning and may even cause implementation of abnormal compensatory motor patterns. There may also be poor compliance. Another limitation of stationary exercises is that they cannot be carried out during activity, as is required for motor learning. Neuromuscular training exercises should instead be carried out under proper biomechanical alignment in which the patient reports reduced or no pain. Exercise should be carried out while performing daily activities. An added plus would be exercises in closed kinematic movements that include weight bearing activities and high numbers of repetitions.
AposTherapy

AposTherapy is a biomechanical therapy that has the ability to combine the two biomechanical treatments for knee osteoarthritis: reducing loads from the affected joint and training of the neuromuscular system. The system is calibrated individually to each individual patient in order to obtain a healthier biomechanical alignment in which less pain is reported and gait patterns are more symmetrical. The patient is then instructed to exercise with the system while performing his or her daily activities at home or at work. This exercise regimen enables the patient to adopt and implement a proper gait pattern without pain. In addition, it has been shown to strengthen the muscles of the knee and improve the timing of muscle activation. Patients also report an increased sense of joint stability.
Centre of pressure – it starts at ground level
The Apos system uses convex adjustable “pods” that are placed under the hind-foot and fore-foot regions of each foot. The elements are attached via a platform in the form of a shoe. This platform enables the clinician to calibrate the biomechanical elements to a customised location for each patient. The ideal location for each patient centres the pressure in the foot to a position that properly aligns the lower limb.
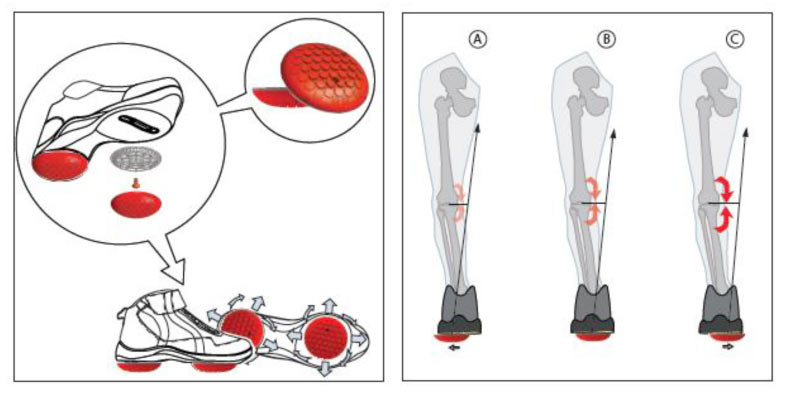
Changing the location of the centre of pressure (COP), through positioning of the “pods”, causes changes in the moments acting on the lower extremity joints. For example, shifting the “pods” to the rear aspect of the foot causes a lateral (backwards) shift of the COP and a decrease in knee adduction moment. This can be seen in Figure 2 (click to enlarge). In addition to proper alignment of the lower limb and a reduction in knee adduction moment, the convex nature of the “pods” promotes controlled perturbation. Since the system can be used during walking throughout the day, the alignment and controlled perturbation are applied repetitively and dynamically throughout all phases of the step-cycle.
Controlling pressure through feet, ankles, legs, pelvis and spine
Studies show that by changing the location of the centre of pressure by shifting the “pods”, the moments acting on the lower extremity, pelvis and spine can be controlled. Similarly, it was shown that the muscle activation patterns also change when the “pods” are shifted.
A significant decrease in pain and improvement in function was observed after nine months of therapy. Furthermore, AposTherapy led to a significant reduction in the peak value and the impulse value (area under the curve) of the knee adduction moment. These results illustrate that, for the first time, a reversal of harm to the knee is achievable.
It is thought that this is the first time that a therapy has led to a significant improvement in the gait patterns of patients with knee osteoarthritis in combination with significant improvements in clinical symptoms. In other words, this is the first time a therapy has been shown to stop the vicious cycle and reverse it.
Conclusion
In conclusion, AposTherapy can improve the pain, function and quality of life of patients with knee osteoarthritis. Furthermore, this therapy has been shown to improve the gait patterns and biomechanical characteristics of knee osteoarthritis that correlate with disease severity, and thus may be able to prevent further deterioration of the disease and instead promote a reversal of the pathology.
A bacterium, virus, or other microorganism that can cause disease.
Full medical glossary






