Ongoing pain after an ankle sprain is common and can be due to peroneal tendon problems. This article describes the range of problems that can affect the peroneal tendons, and the treatment options available, including the role of keyhole surgery.
Peroneal Tendon Injury and Rupture - Contents
- What are the peroneal tendons?
- How are the peroneal tendons injured?
- How do you make a diagnosis?
- What are the treatment options?
What are the peroneal tendons?
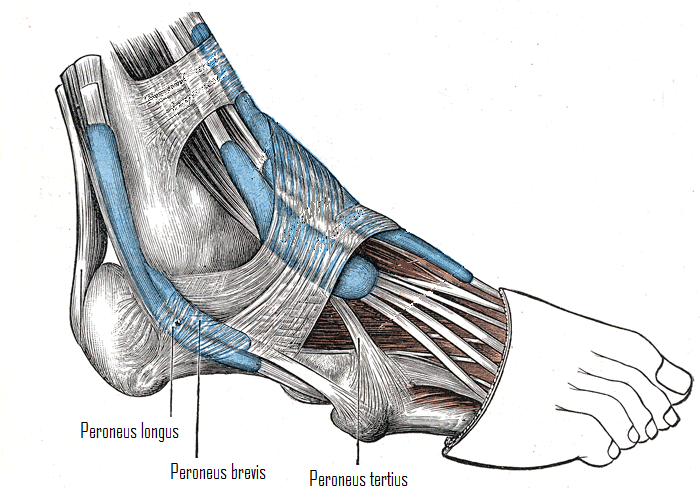
Tendons connect muscles to bones and they help to stabilise and move joints. We have two peroneal tendons, also known as the fibular tendons, which originate from muscles in the outer compartment of the lower leg – peroneus longus (fibularis longus) and peroneus brevis (fibularis brevis). They sit within a groove directly behind the fibula and help to evert (pull up and out) the foot (fig 1; click on image to enlarge). They also act as secondary stabilisers of the ankle joint (the ankle ligaments are the primary stabilisers).
How are the peroneal tendons injured?
Typically the peroneal tendons are injured following an acute twisting injury to the ankle during sport. Injury can also occur if the tendons contract strongly and unexpectedly, such as during skiing. Some people are at higher risk of peroneal tendon injury, such as those people with high arches. Typically these individuals have heels which point inwards and this makes them prone to rolling their ankle, and sustaining both ankle sprains and peroneal tendon injuries (fig 2; click on image to enlarge). In others, the damage occurs slowly over a period of time, due to stress placed on the tendons, or from multiple sprains.
- Injuries can range from tears in the tendons themselves, to damage of the supporting structures which can make the tendons unstable.
- Peroneal tendon injuries are often missed on initial evaluation. If you have ongoing pain after a twisting injury to the ankle, you should seek the help of a Consultant Orthopaedic Foot and Ankle surgeon.

How do you make a diagnosis?
I ask specific questions in clinic and perform a clinical examination. Based on my findings I organise further tests such as an ultrasound scan (USS) or an MRI scan. Often combinations of problems exist and I will formulate a personalised treatment plan with you.
The following three diagnoses are common but have significant overlap.
Tendonitis – this is inflammation of the tendon and its lining. It usually occurs after an injury to the tendon, or from repetitive minor trauma.
Symptoms of tendonitis include:
- Pain
- Swelling
- Warmth to the touch
Tears – these can affect both peroneal tendons, either in isolation, which is more common, or together. They are usually due to overuse or from multiple ankle sprains and occur over long periods of time. These are called chronic tears and the tendons are often thickened as well. Sometimes tears occur acutely due to a twisting injury, and these are called acute tears. In both cases the symptoms are similar to tendonitis as described above. In addition, those with tears sometimes also experience painful clicking.
Subluxation/dislocation – the tendons can slip out of the groove in which they sit. This indicates that the supporting structures, for example the superior peroneal retinaculum (SPR), have been injured. Some patients are more prone to subluxation, resulting from a naturally shallow groove, or from extra bulk within the tunnel where the tendons sit. This can be due to a low lying muscle; usually peroneus brevis or an extra muscle called peroneus quartus. These problems are usually recognised on the USS or MRI scan.
What are the treatment options?
This will be tailored to your individual problem.
In the acute phase after an injury, which is most likely a sprain, you will be treated with Rest, Ice, Compression and Elevation (RICE). Sometimes an Aircast boot for 2–4 weeks can be used to support the foot, and then a gradual rehabilitation programme started. Commonly a problem with the peroneal tendons does not become apparent in the initial phase, and is diagnosed when the symptoms of an ankle sprain do not settle.
Physiotherapy is important from an early stage, whichever type of peroneal tendon problem you have. Muscle strengthening and proprioceptive (balance) training are vital. Sometimes pain hinders this intervention, and if so, early consultation with a Consultant Orthopaedic Foot and Ankle surgeon is vital.
If you have a high arch and are prone to multiple ankle sprains, an insole to rebalance your foot might help. I would refer you to an Orthotist or Podiatrist for an assessment.
What are the surgical options?
If the non-surgical measures above fail and your symptoms are progressive and are affecting your quality of life, I will discuss the surgical options with you.
For peroneal tendon tears, I recommend exploration and repair when possible. Occasionally the tear is too extensive for repair and the diseased portion of the tendon is removed. Both sections of the remaining tendon are then secured to the neighbouring tendon if it is healthy. If both tendons are unhealthy and irreparable, a tendon graft or transfer needs to be performed, although fortunately this is a fairly rare situation.
Peroneal tendon subluxation will often require surgical intervention. The goal of treatment is to stabilise the tendons, whilst maintaining function and preventing ankle stiffness. The lax SPR is tightened and the groove within which the tendons normally sit is deepened. The combination of these two procedures is required to ensure long-term stability. If your ankle ligaments are lax and you have been experiencing them giving way, I will perform an ankle ligament reconstruction at the same time. After surgery, you will require immobilisation for 4–6 weeks in a plaster cast and then begin a structured rehabilitation programme. Ankle stiffness is common in the initial phase, and you will work with the Physiotherapist to regain your movement and strength. Continuing with the proprioceptive (balance) exercises is essential for long-term success of this procedure, as further sprains can make the tendons unstable again.
Are there any new advances?
We are now able to assess the peroneal tendons using keyhole surgery. A small camera is used to visualise both peroneal tendons. Small tears can be treated, but more extensive tears will require an open approach. Only a handful of surgeons are trained to perform this surgery and I currently use this new technology to make an assessment of the peroneal tendons before I perform open surgery. MRI scans do not always accurately detect peroneal tendon tears and using this technology, I can then make a surgical incision accurately over the problem area and keep the incision as small as possible.
I have also developed a technique of deepening the groove where the tendons sit, using keyhole surgery, which does not require a plaster cast following surgery, and allows a faster return to normal function. This technique is successful for a select group of patients with mild tendon instability, but I prefer an open approach for patients with more significant instability.
If you have a peroneal tendon problem, or ongoing pain after an ankle sprain, you should ask your GP to refer you to a Consultant Orthopaedic Foot and Ankle surgeon, like myself, who will make a thorough assessment of your problem.





