This article outlines common injuries in the knee, how these can occur and how these can be treated. This will be of interest to anyone who has suffered from a knee injury and is contemplating surgery.
Contents
- How does the knee work?
- What are knee ligaments?
- The medial collateral ligament
- Anterior cruciate ligament rupture
- Posterior cruciate ligament injury
- Lateral collateral ligament injury
How does the knee work?
The knee is the largest joint in the body, and is made up of the lower end of the femur and the upper end of the tibia, which form a hinge. The hamstring muscles behind the thigh bend the knee, the quadriceps muscles at the front straighten it by pulling on the patella at the front. Unlike the hip joint, there is no inherent stability of the knee from the shape of the bones themselves, and it is made stable by strong ligaments around the joint. If these ligaments are damaged, the knee may then become unstable.
What are the knee ligaments?
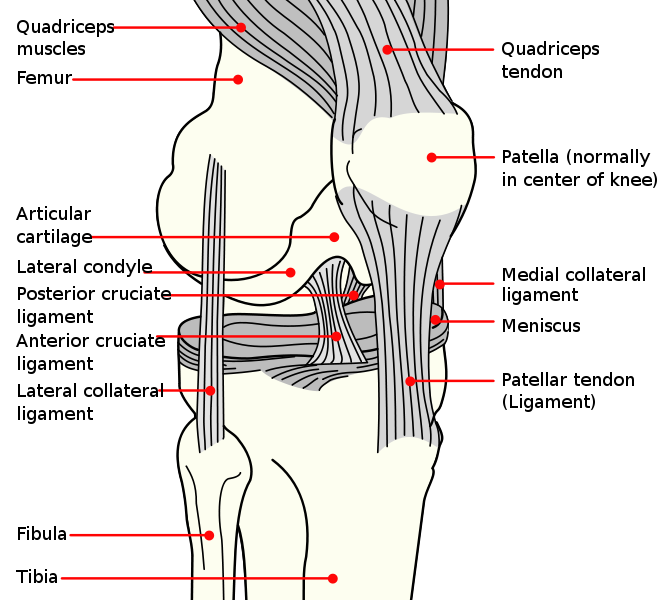
The major ligaments include a thick ligament on the inner (medial) side of the joint, called the medial collateral ligament; the more cord-like ligament on the outer side, called the lateral collateral ligament; and the two ligaments that cross in the centre of the knee, the cruciate ligaments. Of these, one of the cruciate ligaments runs down and forwards in the knee, the anterior cruciate ligament (ACL) and the other runs up and forwards, the posterior cruciate ligament (PCL). There are other restraints and smaller ligaments around the knee, as well as a tough capsule of tissue around the joint. The ligaments can be seen in Figure 1 (click on image to enlarge).
These ligaments do not show up on an x-ray. In practice an orthopaedic surgeon can usually assess the knee by clinical examination, but usually an MRI scan is necessary to confirm the diagnosis.
The medial collateral ligament
Sporting strains and sprains of the medial collateral ligament are common. For example, people playing football may get tackled from the outer side of the leg, which makes the leg bend sideways, opening up the inner side of the knee. Commonly, a ‘pop’ with pain often at the level of the joint will be felt, together with tenderness extending a couple of centimetres down the tibia.
In the majority of cases the ligament is merely sprained, and will heal with a support sleeve or strapping and physiotherapy treatment. Initially this will be ‘range of movement’ and strengthening work, followed by balance exercises. Straight line running can be introduced at four weeks, but it may take six weeks before sport can be resumed. If the injury is more severe it may need six weeks in a knee brace followed by another six weeks of physiotherapy before sport can be resumed. Occasionally the tear is severe enough to warrant surgical repair; usually if it is associated with other ligament injuries within the knee.
Occasionally the ligament does not heal fully, leading to recurrent pain when it is stressed. In this case, ultrasound guided injection therapy with a sclerosing agent (a fluid designed to ‘stick down’ the ligament) is needed, called ‘prolotherapy.’
Anterior cruciate ligament rupture
The classic ACL injury is sustained by rotating on the weight-bearing knee. This is common in skiers where the binding may not come undone in a fall, in footballers who turn awkwardly when being tackled, or in people involved in jumping sports who land awkwardly. There is classically a sudden loud ‘pop’ and the knee collapses. The ACL has a rich blood supply, so the knee often swells rapidly and dramatically within an hour or so. Often it is not immediately too painful, but there is a feeling of instability where the knee will give way on rotational movement.
The initial phase of management of the isolated ACL injury is painkillers, rest, ice (to reduce swelling), compression by an elasticated support bandage, and elevation. This ‘PRICE’ treatment regimen is common for most soft tissue injuries.
The majority of the swelling usually settles within ten days. Provided the joint will straighten, then physiotherapy should be started to strengthen the knee and work on stability exercises. If the knee does not come out straight, then there may be other injuries in the knee such as a tear of the meniscal cartilage, which would need arthroscopy (keyhole surgery) to correct first.
After approximately six to eight weeks of physiotherapy it is usually possible to tell if the knee is going to be unstable or not. In the low demand individual who can regain stability with physiotherapy, further treatment may not be necessary. In the athlete however instability in the untreated ACL tear is common, and will require reconstruction.
Anterior cruciate ligament reconstruction surgery
Unfortunately, merely stitching the ligament back together always fails. The ligament must be replaced by another ligament-like tissue, either the tendons of the hamstrings, or the central part of the tendon below the patella, with a piece of bone at either end (patellar tendon graft, sometimes referred to as ‘Bone-Tendon-Bone’ or BTB). The hamstring method is usually preferable as the scarring is less, and it is sometimes uncomfortable to kneel after patellar tendon surgery. The patellar tendon graft is often reserved for those who manage to tear a reconstructed tendon, or if multiple knee ligaments are injured.
The surgery involves harvesting a length of hamstring tendon that can be done via a small wound on the upper tibia. A tunnel is drilled through the tibia into the centre of the knee at the site of the ruptured ACL, and another tunnel drilled into the femur. The graft is secured in the tunnel in the femur, then tensioned across the knee, and fixed into the tibia, usually by screws or staples. The graft provides initial stability, but it is not at its maximum strength until the body has replaced it with fibrous scar tissue.
There is a risk that the fixation will pull out if the patient falls in the first six weeks, so until muscle control is regained, either crutches or rarely a knee brace may be necessary. Some patients may need crutches for a couple of days; others may have weak quadriceps and as such need a knee brace and crutches for a few weeks.
Rehabilitation following anterior cruciate ligament reconstruction
The rehabilitation from ACL reconstruction requires extensive physiotherapy and home exercise. Initially there will be exercises to get the quadriceps muscles working, followed by weight-bearing exercises (‘closed kinetic chain exercises’) for the first six weeks. The next eight weeks are further gym-based strengthening of the quadriceps and hamstring muscles, with a lot of attention paid to balance and gait. Running is started at four or five months following surgery. Sports that involve involuntary twisting such as football, rugby or martial arts cannot be undertaken until the graft has matured, which takes up to nine months from surgery.
Posterior cruciate ligament injury
The PCL is often injured by hyper-extending over the weight-bearing knee. Classically there is pain at the back of the knee with rapid swelling, and a subsequent feeling of instability.
The ligament either ruptures in its mid-portion or it can pull off a fragment of bone from the upper end of the tibia. The bone fragment should be fixed down using a screw, but the surgical approach requires going through the back of the knee where there are major blood vessels and nerves, and should only be done by highly experienced surgeons.
Most of the mid-substance injuries can be treated by physiotherapy; surgery is much less common than for anterior cruciate injury. If it is needed, then a technique similar to that used for hamstring ACL reconstruction is performed. Often, however, there is a combination of injury to the PCL and to the capsule of the joint adjacent to it called the ‘posterolateral corner’ or a ‘PCL/PLC injury’. In this scenario reconstruction of the PCL both within and from the outside of the knee may be needed.
Lateral collateral ligament injury
The lateral collateral ligament is rarely injured in isolation, unless there is a piece of bone pulled off from the upper end of the fibula. In this case it should be fixed back down either with a screw or wires. If there is a co-existent postero-lateral corner injury then this may also need attention.
PCL, PLC and lateral collateral ligament injuries, whether repaired or not, may need several weeks of treatment in a brace, and extensive physiotherapy before sport can be resumed.





