This article outlines surgery for ankle ligament injuries. This will be of help to anyone who has suffered from a sprain or tear to their ankle ligaments and would like to know what reconstructive surgery involves.
Contents
- What is ankle ligament reconstruction?
- What does the surgery involve?
- What are the risks?
- What happens after surgery?
What is ankle ligament reconstruction?
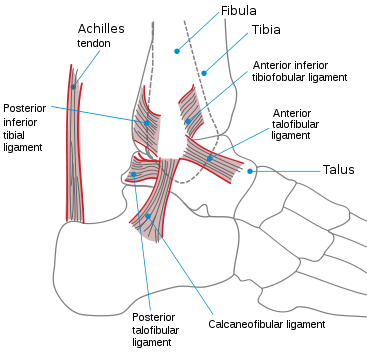
The ankle joint has a large ligament on the inner (medial) side of the joint, and three major ligaments on the outer side, the lateral ligaments. There are other ligaments just above the ankle between the bones of the lower leg, the tibia and the fibula. The ligaments can be seen in Figure 1 (click on image to enlarge).
These ligaments are commonly sprained by twisting injuries, causing pain and swelling. Commonly, ligament injuries respond to a brief period of rest and support from external strapping or bracing, followed by a progressive strengthening and balance retraining regime from a physiotherapist.
Sometimes however, the ligaments can heal slack, leading to recurrent ankle sprains and an unstable ankle joint. If this instability continues, there is a chance of damaging the articular surface lining the ankle joint, leading to premature arthritis.
The most commonly problematic ligaments are those on the outer side of the ankle; these ligaments can be reconstructed to restore stability and function to the joint.
What does the surgery involve?
In many cases the ligaments can be tightened by lifting them off the bone on the outer side of the ankle, and repositioning them with small titanium anchors in the bone (Brostrom repair). In severe or failed cases a tendon from around the ankle can be used to reinforce the repair (augmented reconstruction). A 4 or 5 cm incision is needed, longer for an augmented reconstruction.
If there is evidence of damage to the lining of the joint by pre-operative MRI scanning, then arthroscopy of the ankle can be performed at the same time.
At the end of the procedure a plaster is applied, and the ankle elevated to prevent swelling.
What are the risks?
There may be swelling within the plaster, if it feels tight and painful the cast may have to be split as a matter of urgency to prevent problems with blood flow to the foot.
There are other risks such as numb patches on the ankle or the side of the foot. The exact level of risk is dependent upon a lot of factors; your surgeon should discuss these risks with you before surgery.
What happens after surgery?
Crutches are necessary to keep weight off the plastered ankle for six weeks. The plaster is changed at two weeks to allow removal of the wound sutures, and these are either replaced or changed for a walking boot. Physiotherapy is started during this phase for range of movement, but no running is allowed for at least 12 weeks. Return to sport such as competitive football takes 16 weeks or so.







