This detailed article by a leading neck and throat specialist provides advice for anyone who has discovered a lump in the neck and is unsure what to do. Mr Vaz answers key questions such as " How long should I wait before getting my neck lump investigated?" and "Shouild I have my neck lump removed?"
The most usual cause of a lump in the neck is swollen lymph glands or, more accurately lymph nodes. These are small, pea-sized bundles of white blood cells that form a very important part of the immune system. Lymph nodes are found throughout the body, including a large number in the neck, and they are instrumental in helping to fight off bacteria and viruses.
When one particular part of the body, such as the head or neck, is infected, the lymph nodes near to the site of the infection swell in response and become tender and sore. Typical causes of infection that will cause the lymph nodes in the neck to swell are the common cold, throat infections such as tonsillitis and laryngitis and tooth infections. Viruses, including glandular fever, can also result in swollen lymph nodes in the neck. These infections will normally get better and the lymph nodes will then return to normal.
However, occasionally a lump in the neck that appears to be swollen lymph nodes will be cancerous. For this reason it is important for anyone who has a lump or swelling in the neck that does not appear to be connected to an infection or which has been present for more than a few weeks to see their GP or if associated with the skin - a Consultant Dermatologist.
For more information please read the full article below.
Contents
- How are neck lumps categorised?
- What is a lymph node?
- Should I do something about my neck lump?
- How long should I wait to have my neck lump investigated?
- What investigations should I have?
- What symptoms do neck lumps produce?
- Should I have my neck lump removed?
- Types of neck lumps
- I have a lump on the back of my neck. What could it be?
- I have a lump on the side of my neck. What could it be?
- I have a lump on the front of my neck. What could it be?
- I have a small, pea-sized lump on my neck. What could it be?
- I have a hard lump on my neck. What could it be?
- I have a lump on my neck below my ear. What could it be?
- I have a lump on my neck under my jaw. What could it be?
- I have a tender lump on my neck. What could it be?
- I have a moveable lump on my neck. What could it be?
- What type of doctor should look at my neck lump?
- What is a branchial cyst?
- What is a thyroglossal cyst?
How are neck lumps categorised?
Neck lumps can be categorised in a number of ways. One of these is based on whether they are benign (not dangerous) or malignant. Benign neck lumps are far more common than malignant ones that are usually associated with cancer. The diagnosis of whether a lump in the neck is benign or malignant will be based on medical history, medical examination and special investigations performed on the neck lump. Benign neck lumps can have many causes. The malignant form may originate from lymph nodes and therefore may be as a result of lymphoma or may be secondary to a cancer of the throat. Malignant tumours also arise from the salivary glands.

A second way of categorising neck lumps is based on where they originate from. There are a number of structures in the neck that can produce a neck lump. For example, a neck lump may arise from the thyroid or parotid gland. Of course the most common site of origin is from a lymph node.
What is a lymph node?
Lymph nodes form part of the body’s immune system. They are found throughout the body and there are a large number of them in the neck. They do increase in size when a local infection or inflammation occurs but they can also become enlarged in association with a cancer.
Lymph nodes are designed to mount a local immune response when infection is present. They normally range in size from a few millimetres to a centimetre. It is for this reason that when they are seen in the neck they will have reached a size that suggests either a significant immune response or some other underlying cause.
Should I do something about my neck lump?
The majority of neck lumps are benign, however, as this is not a diagnosis that the general public can easily make I would always say ‘yes’ to this question, especially if the neck lump persists. At the very least your GP should see the lump, however, for a specialist opinion and complete reassurance you may need to be seen by a Head and Neck specialist, preferably, in a Neck lump clinic.
Unfortunately people who do have more worrying malignant neck lumps sometimes take time to accept and come to terms with the idea that they may have a cancer or are in complete denial / scared. It is essential to diagnose tumours as early as possible as an early diagnosis increases the chance of cure in most cancers.
How long should I wait to have my neck lump investigated?
This is a very difficult question to answer. If it is troublesome and worrying to you then I would personally be happy to see you immediately. Current guidelines suggest waiting for a period of 4 weeks with a persistent neck lump. I add caution to this advice and always say that if a neck lump is rapidly enlarging or is associated with other upper-airway /digestive tract symptoms (persistent sore throat, hoarseness, difficulty swallowing or earache) and especially if in a smoker then a more urgent referral is necessary. I as a receiving Doctor would be much happier to see patients sooner rather than later, so as not to delay a significant diagnosis.
What investigations should I have?
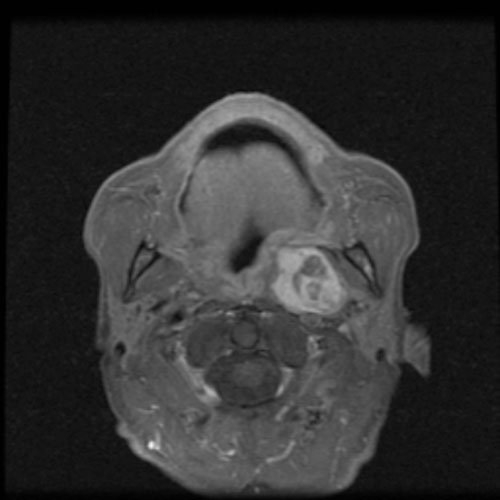
Firstly, a careful medical history should be taken. Then, a thorough examination of the neck, the oral cavity and the upper airway/digestive tract should be performed in the clinic. Following on from this an Ultrasound will usually be performed by the radiologist working as part of the Neck Lump Clinic team. If they feel it appropriate they may sample a few cells from the neck lump, which another doctor, a cytopathologist will look at and interpret. If further imaging is required it will be requested after the initial assessment. Imaging techniques such as CT and MRI Scanning are also undertaken but are tailored to the individual neck lump.
Check with Neck Lump Clinic
What symptoms do neck lumps produce?
Unfortunately neck lumps can be innocuous for quite some time and have no symptoms. As they enlarge they can become tender and can begin to produce some pressure related symptoms. The pressure from a thyroid swelling may produce difficulty swallowing if it is affecting the oesophagus or shortness of breath if associated with tracheal compression.
Some malignant neck lumps that have spread from a tumour elsewhere in the body are associated with symptoms from their primary site such as pain on swallowing, difficulty swallowing, change in the voice or referred pain such as earache. Occasionally malignant thyroid disease may cause damage to localised nerves producing a change in the voice or malignant parotid swellings can cause a facial palsy.
Should I have my neck lump removed?
Not all neck lumps need removal. Many are completely benign and just require a good medical history and examination and possibly an ultrasound to establish the diagnosis. Often benign lymph node enlargement can be left completely untouched. Some recurrent benign neck lumps do require surgical removal if they become recurrently troublesome or if it is essential for a proper diagnosis.
Surprisingly, malignant lymph nodes do not always have to be removed either as there are many ways of treating them. For example, quite a number of squamous cell cancers of the upper airway/digestive tracts are treated with radiotherapy and/or chemotherapy, including lymph node metastasis. If they are to be removed surgically then often a group of lymph nodes is removed in a procedure referred to as a neck dissection.

Types of neck lumps
I have a lump on the back of my neck. What could it be?
It is unusual to have anything serious on the back of the neck. Most lipomas are found in the nape of the neck and may have been present for quite some time. Skin-related pathologies such as cysts may also be found at the back of the neck. Lymph nodes associated with the skin or hair of the scalp may occasionally be found on the back of the neck.
I have a lump on the side of my neck. What could it be?
Lumps on the side of the neck should not be left for much longer than a month without being investigate. These lumps can be benign or malignant and should be treated with suspicion in smokers over the age of thirty.
I have a lump on the front of my neck. What could it be?
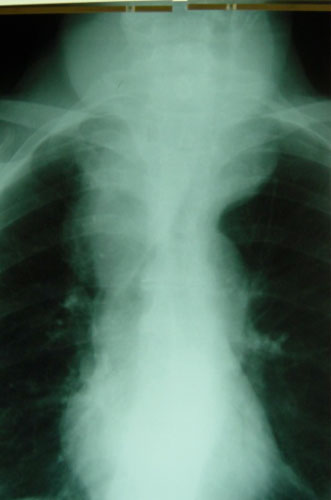
Lumps in the front of the neck may be related to the thyroid gland. Thankfully these are mostly benign but occasionally they can be malignant, warranting an ultrasound. In younger people developmental anomalies related to thyroid descent exhibit as lumps in the front of the neck, known as a thyroglossal cyst.
I have a small, pea-sized lump on my neck. What could it be?
Small lumps are hard to diagnose. If a lump is increasing in size, associated with smoking or upper aerodigestive tract symptoms then it will require urgent investigation. If a lump persists then a history and examination will need to be taken. Position of the lump is also important as it may improve the accuracy of diagnosis through knowing which structure is involved.
See - Rapid access to urgent neck lump clinic
I have a hard lump on my neck. What could it be?
Harder lumps can represent a malignant pathology. If the lump is associated with symptoms such as a change in voice, pain when swallowing or difficulty swallowing and earache then this will require urgent investigation especially when presenting in a smoker. Occasionally inflammatory lumps can present this way also.
I have a lump on my neck below my ear. What could it be?
Lumps just under the ear often represent a lump in the parotid gland. Thankfully most of these lumps are benign but may require surgical intervention. These lumps will require investigation by a Head and Neck Surgeon who uses an expert radiologist and cytologist in order to come to the correct diagnosis and offer the patient an appropriate management plan. Surgery should be undertaken by someone who regularly performs ‘parotidectomy’ as the facial nerve will be close to any lump presenting just under the ear.
I have a lump on my neck under my jaw. What could it be?
Under the jaw, lymph nodes are often associated with infection or inflammation, these lumps are benign. Occasionally malignant lymph nodes from a head and neck cancer or a lymphoma can present in this area. Another cause of lumps under the jaw can be stones causing inflammation and swelling as well as tumours (benign and malignant) arising from the submandibular salivary gland.
I have a tender lump on my neck. What could it be?
Tender lumps will usually represent infective or inflamed areas. This cause should be sought for in a patients history and examination. Thankfully the majority of cases of a tender lump are related to an infective cause, however, patients should be examined and a full history taken to rule out a more worrying pathology.
I have a moveable lump on my neck. What could it be?
Moveable lumps are most often benign. The mobile lump in the neck may represent a lymph node, but it could also be associated with other structures in the neck such as the thyroid, parotid or submandibular glands; these can also represent a pathology that is developmental in its origin. The location of the lump is important as these glandular structures have set positions in the neck.
What type of doctor should look at my neck lump?
Many types of Doctors are qualified to look at neck lumps and will probably do the correct investigations. If there appears to be a significant problem patients are likely to be referred on to a Head and Neck Surgeon. Head and Neck Surgeons have a wide variety of backgrounds. For example, I have an Ear Nose and Throat background but there are also Maxillofacial and Plastic Surgery trained Doctors who have a Head and Neck interest. All Head and Neck surgeons should be able to correctly and efficiently see you in a neck lump clinic and offer the expertise of a Head and Neck Radiologist and Cytologist to help with the specific and accurate diagnosis of neck lumps. I currently run a Friday clinic where patients can come to see me, be examined and then on the same day be further assessed by ultrasound and if necessary samples from the lump can be taken in the form of a fine needle aspiration.
What is a branchial cyst?
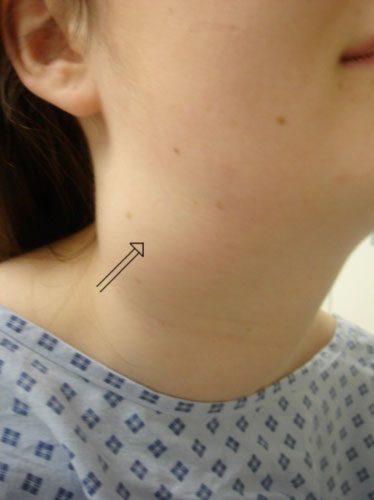
This is a benign neck swelling that usually occurs within the first 3 decades of life. The cyst can rapidly enlarge, especially in association with a flu-like illness and can become quite inflamed. They are investigated with Ultrasound and fluid is often taken from them. In an acute infective state the lump should be treated with antibiotics and left to improve. If this problem is recurrent, the cyst is sizeable or if there is any concern that there may be a more sinister cause then surgical removal should be undertaken. Care has to be taken with a surgical approach as these cysts are often found to lie close to a number of nerves and also to some large arteries and veins.
What is a thyroglossal cyst?
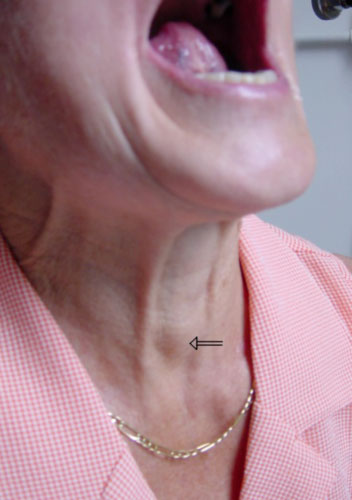
When the thyroid gland forms as the baby develops in the womb it descends from the back of the tongue down to where it sits lower in the neck. The tract caused by this is called the thyroglossal duct and this normally disappears but a cyst may form at any point of this duct formation. This type of cyst can cause repeated swellings in the neck and in these circumstances they require surgical removal. Care needs to be undertaken with any such surgical procedure as it is essential to remove the mid-portion of the hyoid bone, which anchors the tongue in the throat, as without doing this the recurrence rate is significant.
Do I need to see a doctor at the Neck Lump Clinic?
A Rapid Access Neck Lump Clinic allows the immediate assessment of patients with a neck lump to take place. The benefit of this is that it enables those patients whose neck lump is benign to be reassured whilst also allowing for patients with a malignant lump to be swiftly diagnosed so that the appropriate treatment can be rapidly commenced. In addition to this a person who does have a benign neck lump that nevertheless requires surgical input will be seen and managed by a surgeon who specialises in neck surgery.
Click here if you would like further information on rapid assessment via a Neck Lump Clinic



