Contents
- Causes of ovarian cancer
- Symptoms and signs of ovarian cancer
- Making the diagnosis
- Surgery of the ovaries
- Staging of ovarian cancer
- Chemotherapy
- Newer agents in ovarian cancer
- Conclusion
Causes of ovarian cancer
The causes of ovarian cancer are complex and poorly understood. The combined oral contraceptive pill, breast feeding and having children all reduce the risk. However, the inability to have children, difficulty in falling pregnant, never having being pregnant and fertility treatment all increase the risk of ovarian cancer. Genetic factors such as faults in the BRCA gene account for 5% of cases of ovarian cancer. The likelihood of having a fault in the BRCA gene is increased in those women who have family relatives with breast and ovarian cancer. Relatives of women with breast and ovarian cancer may wish to discuss their risk of developing the disease with a geneticist and/or may wish to consider undergoing risk reducing surgery (removal of the tubes and ovaries).
Symptoms and signs of ovarian cancer
Ovarian cancer is often referred to as the “silent killer” as there are rarely any symptoms before the cancer spreads beyond the ovary. This means that by the time medical help is sought over 75% of women will have advanced disease. Some women may be aware of a lump in the tummy which may be uncomfortable. However for most women the changes are subtle - an expanding waistline despite a loss of appetite, weight loss especially noticeable on face and limbs and bloating - symptoms often erroneously attributed, by the patient, to the change in life (i.e. menopause). The most common symptom of advanced disease is abdominal pain. Some women may experience a change in bowel habit –new onset constipation or diarrhoea often resulting in a referral to a bowel specialist.
Making the diagnosis
A thorough history and clinical examination including a vaginal examination is essential. Initial investigations include an ultrasound scan (USS) of the abdomen and pelvis and a Ca125 blood test, which tests for the presence of a particular protein. The Ca125 blood test is abnormal in 50% of early ovarian cancers and in 80% of those with advanced disease. An abnormal Ca125 and an abnormal USS should prompt a referral to a specialist cancer gynaecologist who will then arrange a CT scan of the chest, abdomen and pelvis to look at the extent of the disease. All the scans and the other tests are then discussed by a team of experts including the surgeons and doctors specialising in chemotherapy (oncologists) and a decision reached regarding further treatment. The treatment options will include an operation to remove the cancer followed by chemotherapy or chemotherapy first to shrink the cancer and surgery after 3 courses of chemotherapy.
Surgery of the ovaries
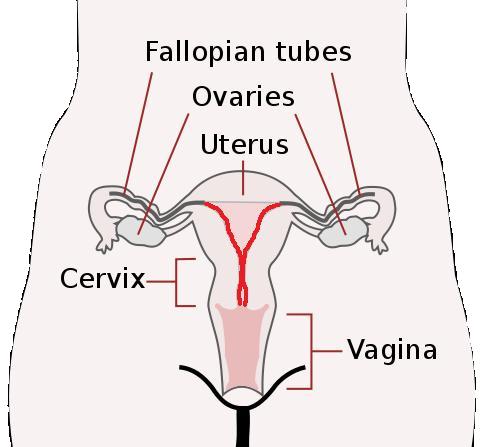
The aim of the surgery is two-fold – to remove the cancer and to “stage” the disease. Staging refers to the extent of the disease and is outlined further in the table below. In early stage disease the aim is to remove all of the cancer and to take samples from other tissues. This will usually involve an omentectomy (removal of fatty tissue that overhangs the bowel), a hysterectomy and removal of the fallopian tubes and both ovaries. However in younger women with cancer confined to one ovary it may be possible to leave the other ovary and tube and the womb. In this situation the woman retains the ability to fall pregnant in the future. This however should only be undertaken by an experienced cancer gynaecologist following a full review of the case by the team of experts.
When the cancer has already spread outside the ovary then the aim is to remove all of the cancer including both the ovaries and tubes and the womb. In some cases this may be easier to achieve following chemotherapy first to shrink the disease.
Staging of ovarian cancer
| Ia | cancer in one ovary |
|---|---|
| Ib | cancer in both ovaries |
| Ic | one or both ovaries with cancer on the outside or fluid in the belly |
| II | cancer spread to the tubes or the womb |
| III | cancer spread into the belly |
| IV | cancer spread into the liver or the lungs |
Chemotherapy

Chemotherapy or drug treatment is a very important part of the treatment of ovarian cancer. In most cases the patient attends the hospital for a few hours and returns home afterwards. The drugs are usually given into a vein in the hand over a course of a few hours. During this time the patient can eat and drink. It is usual to see a doctor or a specialist nurse and a pharmacist on each occasion before the treatment is given. This provides an opportunity to ask questions and to report any concerns/side-effects since the last visit.
Platinum-based chemotherapy remains the current gold standard in this disease. In most cases the platinum drug of choice is carboplatin but cisplatin is an equally effective drug but with a different side effects. Carboplatin is usually given alongside paclitaxel (taxol). Some patients may not be fit enough to receive both drugs and may be treated with carboplatin alone. Currently these drugs are administered once every three weeks for a maximum of six treatments or cycles. However a new clinical trial will investigate whether giving the drugs weekly is more effective.
There are also clinical trials assessing other ways of delivering the drugs such as directly into the belly via a tube. These options may, if appropriate, be discussed by the cancer specialist.
The side effects of chemotherapy vary with the drugs used. Most chemotherapy drugs cause nausea and vomiting but this is usually very well controlled with anti- sickness medication - which is given intra-veneously before the chemotherapy and in tablet form to take home. Patients on chemotherapy are also more susceptible to infection and are therefore advised to report to their local hospital should they develop a fever or become unwell. With the two drug treatment, pins and needles in the fingers and feet is common and can become more pronounced during the course of the treatment It usually resolves slowly over weeks to months following completion of the treatment. It is also not uncommon to experience muscle aches and pains in the legs and arms. These usually only last for a few days and may be helped by codeine and paracetamol. Temporary total body hair loss occurs with the paclitaxel. Some patients may experience an allergic or hypersensitivity reaction to one or other of the drugs during the treatment and therefore patients are observed carefully during the treatment.
Newer agents in ovarian cancer
Despite surgery and chemotherapy, three out of four women who are treated for cancer that has spread beyond the ovary will sadly die from ovarian cancer. Thus, there is a great unmet need for more effective treatments for this cancer. This has focused attention on understanding how the cancer grows and spreads and on developing new drugs.
The growth and spread of a cancer is dependent upon the development of a blood supply. A number of factors have been identified that are critical to this process. These growth factors can be switched on by the cancer thereby permitting it to develop a blood supply and with it the ability to grow and spread. Switching off or blocking (inhibiting) this process may slow down the cancer growth. One such inhibitor is bevacizumab (Avastin). This agent is given intravenously during the chemotherapy and as maintenance treatment after the course of chemotherapy is completed. Recently completed clinical trials suggest that this drug is effective in slowing down the cancer recurrence but it is not yet known whether it will result in more women living longer than they would without it. Other agents under investigation include AZD2171 (Cediranib) which can target a number of these growth factors and has the advantage of being administered as a tablet.
The side effects of these agents differ from conventional chemotherapy drugs. These include an increased risk of bleeding, bowel damage, high blood pressure, kidney damage and skin rash.
It is impossible to say whether any of these agents will increase cure rates in ovarian cancer but it is possible that by incorporating these agents into our current treatment we will succeed in keeping more women alive for longer than we do at present.
Conclusion
The treatment of ovarian cancer is becoming increasingly complex with the emergence of new agents and different chemotherapy schedules. Complete removal of all visible cancer by an experienced cancer gynaecologist and assessment by a specialist ovarian cancer doctor is critical to patient outcome. It is therefore imperative that women with ovarian cancer are managed by a team of doctors with expertise in this disease.
Dr McCormack offers this advice to women attending a medical appointment for ovarian cancer:
Make a note of any questions that you have before your appointment. Take a friend with you as there is lots of information to take in. Take a pencil and paper and expect to receive lots of written information. If this is not offered ask for it!
For further information on the author of this article, Consultant Clinical Oncologist and Gynaecologist, Dr Mary McCormack, please click here.
The time of a woman’s life when her ovaries stop releasing an egg (ovum) on a monthly cycle, and her periods cease
Full medical glossary



