Total Health asks ten top hip Consultant Surgeons the following questions:
-
Q1: Which type of hip prosthesis do you routinely use and why?
-
Q2: How long have you used this choice of hip prosthesis?
-
Q3: Do you use this prosthesis exclusively?
-
Q4: If you sometimes use alternative prostheses please specify which type(s) and why?
-
Q5: What procedure do you use?
-
Q6: If you needed a hip replacement now which prosthesis and procedure would you opt for?
-
Q7: What over-riding piece of advice would you give to someone considering having hip replacement?
See also answers from the following hip replacement experts:
- Mr Phillip Stott
- Miss Samantha Tross
- Mr Howard Ware
- Mr Ed Davies
- Mr Winston Kim
- Mr Charles Willis-Owen
- Mr Mark Rickman
- Mr Jeremy Latham
- Mr Paul Jairaj
- Mr Stephen Jones
- Mr Warwick Radford says:
Q1: Which type of hip prosthesis do you routinely use and why?
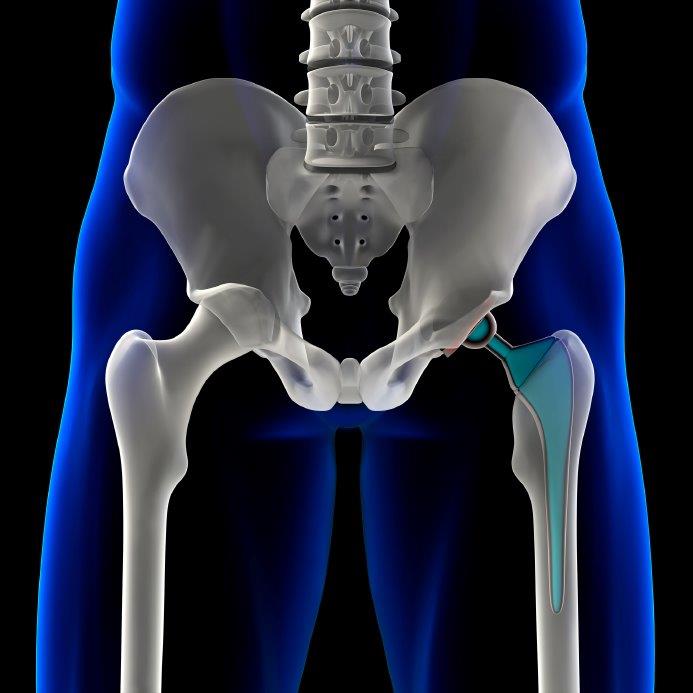
"Hip replacements can be fixed to bone with cement or without using cement. For younger patients who are very active (say up to the age of 60), I use uncemented components with a ceramic on ceramic bearing. These uncemented components are coated with hydroxyapatite which is chemically similar to bone so that the bone grows directly onto the metal surface. Once bonded, (which takes about six weeks), it is unusual for it to fail later on. On the rare occasion that this does happen, it is a relatively straightforward procedure to revise the implant as there is no cement to remove."
"I use a 36mm diameter ceramic ball on top of the titanium femoral component, which articulates with a ceramic liner inside the shell of the new titanium socket. Ceramic is the hardest wearing substance available for hip replacement and microscopic debris (which is shed by all hip replacements) rarely causes adverse reaction in the soft tissues. Modern ceramics are extremely tough and durable and the risk of the brittle ceramic fracturing is negligible. The only downside to a ceramic on ceramic bearing is there is a small incidence (1% or 2%) that it may squeak. This may be due to component orientation but it can occur with any ceramic on ceramic hip. However, it is usually an intermittent problem and I have never known a patient to request revision for a persistently squeaking hip. This potential side effect is greatly outweighed by the durability of the bearing surface."
"The uncemented ceramic on ceramic hip I use for younger patients is made by a Swiss company called Symbios. This company offer surgeons the use of pre-operative planning from CT scans, which is extremely accurate in predicting size of components and aids positioning. This pre-operative planning is important and the Symbios system is the most accurate currently available. This restores anatomy so that hip muscles are balanced and can work efficiently, improving function and stability (i.e. less likely to dislocate)."
"For older patients I use an uncemented socket and a cemented stem made by Stryker, one of the leading American implant makers. I use their uncemented Trident titanium socket with their highly durable polyethylene liner. On the femoral side I use the Exeter cemented stem which is a British design, more than 40 years old and is one of the top three cemented femoral components. A 36mm diameter ceramic ball is placed on top to articulate with the polyethylene liner."
"It is interesting to note that if someone is 63 years or older, then their hip replacement is statistically likely to outlive them."
Q2: How long have you used this choice?
"I have been using the Symbios hip for about seven years and the Stryker Trident/Exeter combination for at least ten years."
Q3: Do you use this prosthesis exclusively? If not, please indicate the approximate percentage that you perform using it.
"I stopped using metal and metal (resurfacing) hip replacements in 2010 when concerns were raised regarding local tissue reaction to metal ions. No-one ever demonstrated any significant functional advantage over more conventional hip replacements. I now only use Symbios or Stryker hips and tell my patients they may do whatever they like with their new hips providing it feels comfortable."
Q4: If you sometimes/regularly use alternative prostheses please specify which type(s) and the approximate percentage of procedures carried out with each.
"The only alternative to the standard hip replacement I use is a custom stem for patients with unusual bony anatomy or congenital hip problems. Custom femoral components are similar to their off-the-shelf counterparts but are specifically tailored to fit precisely within the femoral canal and to restore anatomy and optimise function. These are again made for me by Symbios, one of only a few companies to offer this service. They started in 1989 for the European market, and more than 28,000 have been implanted. They were made available in the UK in 2007 and around 400 have been inserted since then."
Q5: What procedure do you use? If you take a different approach from the norm (e.g. minimally invasive surgery, computer-navigated surgery, patient-specific etc), please explain what you view as the benefits of your particular chosen specialism.
"Regarding minimally invasive surgery, this became fashionable several years ago but I have never regularly carried this out as in my opinion the most important objective in replacing a hip is to position and orientate the components correctly. This requires adequate access and I therefore use an appropriately sized incision, rather than a cosmetically smaller incision that could risk compromising positioning."
"Several years ago I helped a company develop their computer navigation system, although I have not adopted this method. It aids the surgeon in positioning the components but if not set up properly it can mislead, and for me clinical judgement will always be the overriding factor. It also adds about 20 minutes to the procedure time, which normally takes less than an hour. Another recent move is to use the direct anterior approach to the hip joint, which is said to speed up recovery. The more commonly used approaches in the UK are the anterolateral approach or else the posterior approach. I use the latter. I have visited surgeons who use the direct anterior approach, which has a certain elegance in that it passes between muscle planes, but the access is not as good and the procedure takes considerably longer to set up and carry out. I am yet to be convinced that this offers any significant advantage over the posterior approach. I have had three patients leave hospital the day after surgery, and, as someone once said to me “why would you want a scar you can see?” (The posterior scar is mostly over the buttock)."
Q6: If you needed a hip replacement now which prosthesis and procedure would you opt for?
"I would hope my surgeon would use a ceramic on ceramic bearing as I am still relatively young and active. I would be happy if it was uncemented and would want components which are tried and tested. However, ultimately I would be guided by the recommendation of my treating surgeon."
Q7: What over-riding piece of advice/reassurance/guidance would you give to someone who is apprehensive about their need for hip replacement?
"Hip replacements are to improve quality of life. It is one of the most successful operations in the whole of surgery. The vast majority of patients are delighted with the result. Surgeons do everything to minimise risk and you will be told about these measures when you sign your consent form. I would recommend seeing a competent and experienced hip surgeon and be guided by them regarding what is the appropriate implant for you. I would suggest avoiding anything but rudimentary research on the Internet. There is enough information out there to enable you to do a hip replacement yourself, although you won’t have had the years practice. It is also an environment for marketing and some advice is overplayed and can be misleading. If you have any questions, best to ask you surgeon."
See also answers from the following hip replacement experts:
- Miss Samantha Tross
- Mr Howard Ware
- Mr Ed Davies
- Mr Winston Kim
- Mr Charles Willis-Owen
- Mr Mark Rickman
- Mr Jeremy Latham
- Mr Paul Jairaj
- Mr Stephen Jones












