This article describes Uterine Fibroid Embolisation (UFE), a non-surgical procedure for treating uterine fibroids. This will be of interest to any woman looking for an alternative to a hysterectomy or myomectomy for large fibroids.
Contents
- Introduction to Uterine Fibroid Embolisation (UFE)
- Before UFE
- The procedure itself
- Common concerns
- What happens straight after UFE?
- How long will it take me to get back to normal life?
- How quickly will I start to feel the benefits?
- Follow-up after UFE
- Are all fibroids suitable for UFE?
- What are embolic agents?
- Optisphere (Gel-BEAD) bio-degradable spheres
- PVA
- Embospheres
- Bead Block
- Embozenes
- What are the benefits of UFE compared to other treatments?
- What are the possible complications of UFE?
- Fertility after embolisation
- Having UFE on the NHS
- Having UFE privately
- UFE for the overseas visitor
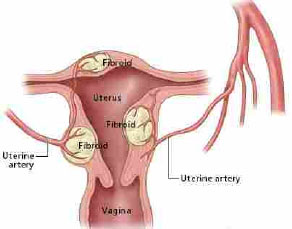
Introduction to Uterine Fibroid Embolisation (UFE)
This is a non-surgical, minimally-invasive, procedure that blocks off the arteries that supply the fibroids with blood (the uterine arteries), therefore shrinking the fibroids.
- It is performed with the patient conscious, but sedated.
- It is carried out by an Interventional Radiologist (IR), a doctor who has been specially trained in using X-ray equipment, interpreting the images produced and performing operations using X-ray or other modern imaging equipment for guidance.
- It was first performed in France in the early 1990’s, although radiologists have been embolising uterine arteries for more than 20 years to control bleeding from the womb, especially after childbirth.
- 80-96% of women are satisfied with the treatment and its result, and most patients rate the procedure as “very tolerable”.
- The shrinkage in fibroid size averages 60% but varies from 20-100%.
- Most women start getting relief of symptoms immediately, although fibroids that have taken years to develop will take months, or even years, to shrink to their final size.
- Over 300,000 women world-wide have undergone uterine fibroid embolisation (UFE).
Before UFE
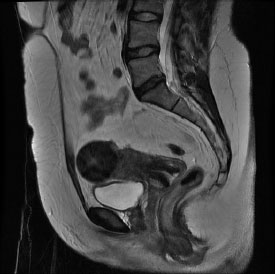
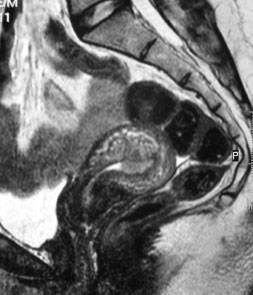
- You will have an ultrasound, and an MRI scan, to determine whether your fibroids are suitable for embolisation.
- You will be pre-assessed by Dr Hacking and your gynaecologist.
- You will be admitted to the ward or Day Case Unit (DCU) on the day you have UFE performed.
- You should not eat or drink for at least 4 hours before the procedure. You may be given an intravenous drip (into a vein) to avoid dehydration.
- You will need to shave both sides of your groin.
- You will be given an antibiotic tablet and a Voltarol suppository to prevent infection and help with pain relief.
- You will need to put on a hospital gown.
The procedure itself (see Fig 2)
- You will be taken on a trolley from your ward, or walk from the DCU, to the Interventional Radiology procedure room or ‘Cath Lab’, where you will lie flat on your back on the X-ray table.
- If you are anxious you will be given relaxing injections through a cannula in a vein in your arm. Intra-arterial local anaesthetic and pain-killing injections (Morphine) will be given during the procedure to control anticipated pain expected as a result of fibroids dying within the first hour after the procedure.
- A device to monitor your oxygen levels and heartbeat will be placed over your finger.
- A blood pressure cuff will be wrapped around your arm and will automatically tighten and record your blood pressure every 5 minutes.
- You will be given oxygen through small tubes up your nose if sedated.
- The skin over your groin and surrounding areas will be cleaned with Iodine antiseptic (or Chlorhexidine, in the case of Iodine allergy).
- Surgical drapes are applied over your body with a small window left over the right side of the groin.
- A local anaesthetic is injected into the groin or wrist if a radial approach is preferred.
The procedure can be performed from either the groin or the wrist. This will be discussed and planned in advance.
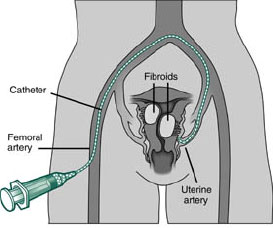
Groin Approach: The Interventional Radiologist (IR) feels for the arterial pulse and then makes a minute nick (around 1mm), in the skin over the right side of the groin, and inserts a needle into the artery. Once in place, a sterile guide wire is placed through the needle into the artery. The needle is withdrawn, allowing fine plastic tubes (a sheath and catheter) to be placed over the wire and into the artery. (see Fig. 3)
Radial (wrist) approach: An Ultrasound guided puncture is performed after local anesthetic is administered. A cocktail of drugs is injected to prevent spasm occurring and then a small calibre sheath is advanced into the radial artery. The embolisation itself is very similar with either approach and will be described in the following section. At the end of the radial procedure a compression device is applied to the wrist and mobilization can commence very soon afterwards.
The arterial catheter is steered to the arteries feeding the uterus using X-rays to see where it is going. X-ray dye (contrast medium) is injected down the catheter into the uterine arteries (this will feel hot, but is not painful). Once the uterine blood supply has been established, tiny plastic or Gelatin sponge particles or spheres, like tiny grains of sand or wallpaper paste, are injected through the catheter into the uterine arteries.
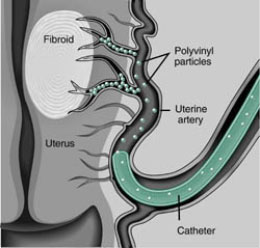
These particles block the blood vessels supplying the uterus and fibroids and get wedged there, causing the cells within the fibroid, but not the uterus, to die. The uterus is very resistant to temporary loss of blood and will receive an alternate blood supply within minutes from other surrounding arteries. (see Fig 4.) Local anesthetic is injected directly into the uterine arteries which has led to a significant improvement in short term pain control iin the 4-6 hours after the procedure.
Both the right and left uterine arteries need to be blocked in this way. Usually it can all be done from the right groin. Some Radiologists prefer to perform the procedure using separate right and left groin punctures and a radical approach technique is gaining popularity, but gives no better results than from a groin approach.
The procedure finishes when there is no more blood flow into the fibroid. The catheter is withdrawn and the IR or nurse presses on the groin puncture site to prevent bleeding and then may put a small elastoplast over the wound.
On average, the procedure takes about 30 minutes.
Common concerns

What happens straight after UFE?
- You will be taken back to the recovery area or DCU on a trolley where you will be looked after by nurses who will take your pulse and blood pressure and check the wound.
- You will need to lie still in bed for a few hours to reduce any chance of bleeding from the groin.
- Most patients experience some degree of pelvic pain. This ranges from very mild to severe, crampy, period-like pain. This severe pain has been much better managed recently by the introduction of intra-arterial local anaesthtetic injections performed during the embolisation itself. Post procedural pain is further controlled with a cocktail of strong painkillers, which you will give yourself through the cannula (PCA - Patient Controlled Analgesia) that was inserted in your arm before the procedure as well as anti-cramping and anti-sickness drugs. The pain is worst in the first 8-12 hours. After intra arterial local anaesthetic many women experience little pain for the first 4-6 hours and when this anaesthetic wears off the degree of pain is significantly less and easier to manage.
- The painkillers and sedatives may mean that you sleep for a few hours afterwards.
- The drip and PCA will be discontinued the following morning to be replaced by the same cocktail of drugs in tablet form.
- Most women stay in hospital for one night, although if you do need to stay in longer than a day, this is not a problem.
- Most patients get a slight fever after the procedure. This is normal and is a good sign as it is due to the fibroid breaking down. The anti-inflammatory painkillers will help to control this fever.
- The pain will probably still be present when you go home. You will be given painkillers to take home with you and you should rest for 3-4 days, drink plenty of fluids and stay as mobile as you can.
How long will it take me to get back to normal life?
- Women can go back to normal activities, including sport and sexual activity, as soon as they feel able.
- Unlike most surgery, there is no muscle-cutting involved in UFE, so you are not at risk of bursting a wound or causing a hernia.
- In order to avoid infection, it is advised that you do not use tampons or swim in non-chlorinated water if you have a discharge.
- Most women are ready to go back to work after 3-14 days. It is probably best to allow for being off work for a fortnight.
How quickly will I start to feel the benefits? (see Figs. 5a & 5b)
- Immediately after UFE, the fibroids become soft.
- Pressure symptoms on the bladder and bowel and heavy periods usually respond within days.
- Average fibroid volume reduction is 40% at 3 months, and 60% at one year.
Usually an ultrasound scan is performed after 1 month and an MRI scan after 3 months, and again a year after the procedure. If there is cause for concern or any worrying side effects earlier scanning can be performed.
Are all fibroids suitable for UFE?
- It is usually the position, blood supply and location of fibroids that determine success.
- The richer the blood supply to the fibroids, the better the response.
- Submucus fibroids respond best, although intramural and sub-serosal ones also respond well.
- Pedunculated fibroids (those with a stalk) can be successfully embolised as long as the width of the stalk is not too thin in relation to the size of the fibroid.
- UFE can be combined with myomectomy using hysteroscopic, laparoscopic or abdominal routes to combine the success of these two complimentary treatment options.
- They are the particles used to block the uterine arteries.
- There are various different types, some of which dissolve and others which remain in the body.
- They can never be ‘dislodged’. Vigorous exercise, which increases the heart rate and therefore blood flow, will only jam the particles further into the blood vessel.
- Tiny blood vessels in the uterus remain intact and keep the womb alive, while the fibroids, which are far more susceptible to a shortage of blood, die.
- As yet, none of these embolic agents (listed below) has been proven to be more effective than the others.
- 1mm thick sponge is cut up into approximately 1mm cubes. This is dissolved in X-ray contrast agent to produce a slurry like wallpaper paste.
- This is likely to block large and medium-sized uterine arteries, but leaves smallest arteries patent to allow maximum blood supply to the normal uterine tissue.
- It dissolves in a few days or weeks, but completely ‘dead’ fibroids cannot regrow.
- It has been in common use for over 20 years. It is more likely to leave the uterine arteries blocked than the other agents.
- It may cause less post-procedural pain than PVA and other agents.
Different sized particles are used, usually 0.3-0.5mm or 0.5-0.7mm in size. In theory, these will block arteries down to these sizes, but in reality particles clump together to block the arteries, for example, if three 0.5mm particles clump together, they will block an artery of 1.5mm diameter. The level of arterial blockage may be similar to that seen with Spongistan slurry. The uterine arteries are more likely to re-open within 3 months.
This has also been in common use for over 25 years and is the most common agent used in the UK.
The first of the ‘Spherical’ embolic agents, these are 0.5-0.9mm non-dissolvable particles. They do not clump and therefore block arteries at a smaller diameter. The main uterine arteries usually remain open, but less than with Embozenes, Beadblock or PVA.
Blue coloured spherical PVA, commonly used in 0.7-1.2mm sizes. Less likely to permanently block uterine arteries, but may be less effective than the other agents in killing all the fibroids.
Colour coded Polyzene-F coated spherical embolic. Used in 0.7-1.3mm sizes. Leaves arteries open and is as effective as PVA, Embospheres and Gelatin sponge.
Optispheres (Gel-Bead) Bio-degradable Spheres
The newest embolic agent available and being trialled in 2017 and 2018. A Gelatin microsphere which potentially combines the advantages of a spherical agent getting deep fibroid penetration and so effectively ‘killing’ all fibroids with being a non-plastic, biodegradable agent allowing full uterine artery patency and preservation of both ovarian and uterine function to allow improved fertility outcomes. Results of trials performed by Dr Hacking due in 2018

What are the benefits of UFE compared to other treatments? (See Figs. 6a & 6b)
- No scar.
- Treats uterus up to and above the umbilicus.
- Treats heavy periods with anaemia without surgery.
- You retain your uterus.
- There is no cutting and therefore no stitches nor scar.
- No blood transfusion is required.
- The likelihood of fibroids growing back is only around 20- 25% five years after treatment, much lower than after myomectomy.
- Only 1-2 nights in hospital.
- Approximately two weeks off work, often less.
- No general anaesthetic required and you are conscious throughout the procedure.
- If further treatment is necessary, myomectomy is a more successful operation if UFE has been performed first as the chance of uncontrollable bleeding, which can lead to hysterectomy, is much less likely.
What are the possible complications of UFE?

There are risks attached to every medical procedure. The important thing is to weigh up the benefits of being treated against the risks of a rare complication happening to you. The risks of fibroid embolisation include:
- Deaths have occurred with hysterectomy and myomectomy. Usually mortality figures of 1 in 1,500-3,000 for these two surgical techniques are quoted.
- Death following UFE has been reported in 5 cases worldwide due to severe infection in 2 cases, pulmonary embolus in 2 others and unexpected shunting and multiple organ embolisation in a 5th case. This is from a total of between 150,000 and 200,000 cases performed worldwide, giving a mortality of 1 in 30,000 - 40,000.
- It must be stressed that risk of death is very rare in any of these procedures.
- True uterine infection is very rare, probably less than 1 in 1,000.
- More commonly dead fibroid material can become lodged in the uterine cavity and if untreated can become infected. Signs of this include an unpleasant, foul smelling discharge, pain and fever.
- This can often be predicted after embolising large submucosal or intracavity fibroids and can happen at any time up to 9 months after UFE. Detailed advice will be given to the patient, her Gynaecologist and GP about this possibility. The Interventional Radiologist should be contacted urgently to arrange antibiotics and scanning and if appropriate an urgent Gynaecological assessment.
- True uterine infection will require antibiotics and probably urgent hysterectomy, but usually the uterus is intact and if the problem is one of fibroid passage then antibiotics and pain killers will usually suffice, and if not delivery of the fibroid by the gynaecologist or hysteroscopy with fibroid clearance will usually be possible.
- Your Interventional Radiologist will ask you before UFE whether you would have a hysterectomy if your uterus became infected. If you would not, under any circumstances, then your radiologist is likely to advise you not to undergo embolisation.
Ovarian failure / premature menopause
This is due to accidental embolisation of the arteries to the two ovaries and is often the result of different arrangements of blood vessels in some patients. The greater the experience your Interventional Radiologist has and the use of larger embolic particles has made this complication very unlikely. The chances of premature menopause are less than 2% under the age of 45, rising each year up to around 15% at age 50. About 3 times as many patients have no periods for a month or two after UFE.
Embolisation with temporary or biodegradeable embolic agents such as Optisphere (Gel-Bead) and Gelfoam slurry are less likely to cause ovarian failure than with more permanent, especially smaller (<500micron size) ‘plastic’ embolics.
Passing a fibroid through the vagina

This happens in approximately 3-4% of all patients and usually occurs 6 weeks - 3 months afterUFE. It is most common with submucous fibroids, particularly if largely intra-uterine. Fibroids can either pass in large pieces or break up and pass unknowingly. The MRI scans in these cases can show a remarkably normal uterus on follow up imaging.
After passage of a fibroid and before you attempt prior to become pregnant, it is wise to have a hysteroscopy to observe if there are any significant intrauterine adhesions present, and treat if necessary.
This happens in about 4% of patients and is usually due to the fibroid breaking down. It normally lasts for around 2 weeks, though can go on intermittently for several months. If it is accompanied by fever, you should contact your Interventional Radiologist and Gynaecologist as soon as possible. You might need to have an internal exam to make sure the dead fibroid has not fallen down into the vagina or become stuck in the cervix, as this could cause infection.
Haematoma (bruise around entry point)
A small bruise in the groin or wrist if a radial approach was used is quite normal, but if it becomes bigger, it may need treating with antibiotics to prevent infection.
Fibroids fed by an additional blood supply (usually the ovarian arteries)
This happens in about 5 - 10% of cases. The ovarian arteries can be embolised. Using smaller ‘plastic’ embolic particales this is more likely to result in premature menopause if both ovarian arteries are blocked. The risks of Ovarian failure seem much lower using larger (>700micron) ‘plastic’ or either Gelfoam Slurry or the newer Optisphere (Gel-BEAD) dissolvable embolics. This option can be considered for women after discussion in womenwho have no further fertility wishes or whose fibroids are unlikely to be dealt with using uterine artery embolisation alone. Your Interventional Radiologist will talk to you about such wishes if it is found that the ovarian arteries are supplying the fibroids with blood.
Fertility after embolisation
The average age of women undergoing UFE is around 40, so natural fertility is already starting to decrease, even without the fibroids.
The Royal Colleges of Radiology (RCR) and Royal College of Obstetrics and Gynaecology (RCOG) currently advise women wanting to get pregnant, to obtain myomectomy for a large single or a small number of fibroids especially when they are subserosal or intramural. When they are small and submucosal or intracavity hysteroscopic myomectomy is preferable in experienced hands. UFE is probably now an acceptable alternative with large or particularly multiple fibroids and can be combined with myomectomy.
There is growing evidence that UFE may indeed be superior to open myomecomy in young women with multiple fibroids. Treatment success is high and fibroid recurrence rates are lower compared with myomectomy. Women can carry pregnancies after UFE, although unfortunately miscarriages do still occur. A woman carrying a pregnancy to full term may have a vaginal or natural childbirth after UFE whereas a caesearan section is usually advised in women who have undergone abdominal myomectomy. More and more studies have shown that ovarian function, as measured by the Anti-Muillerian Hormone levels is not adversely affected by the UFE procedure. The use of dissolvable Gel-Bead embolics agents raise the possibility that uterine function may be better maintained compared with other embolic agents although these claims are as yet unproven.
There have now been over 300 successful pregnancies after UFE.
Having UFE on the NHS
An increasing number of centres are now offering UFE. This is a technique with quite a long learning curve and so experienced operators should be sought out wherever possible. For UFE at Southampton you will need a referral to an Interventional Radiologist from either your GP or your gynaecologist. If you wish to see an Interventional Radiologist out of your geographical area, you will need to ask the doctor who is referring you to obtain funding from his PCT.
Having UFE privately
All private insurance companies now cover for UFE. MRI scans will usually be charged on top of the usually quoted figures. UFE is available by Dr Nigel Hacking at a number of hospitals in Southampton, Trinidad and London.
UFE for the overseas visitor
A number of institutions will now quote for overseas patients. Travel arrangements and full costs should be included wherever possible. To arrange an appointment with Dr Nigel Hacking please click here.
The time of a woman’s life when her ovaries stop releasing an egg (ovum) on a monthly cycle, and her periods cease
Full medical glossary



