Introduction
Faecal incontinence is a major social problem affecting between two and 15% of the population. The condition is known to increase with age and it is estimated that 16% of men and 26% of woman above the age of 50 years will suffer from faecal incontinence. The cost implications for managing this condition in the community is considerable, with up to £100 million spent each year on incontinence pads, plugs or absorbents.
Contents
- What is faecal incontinence and what are the causes?
- Common symptoms
- Diagnosing the condition
- Treatment and recent advances
- Artificial Bowel Sphincters
- Neosphincters
- Colostomy
-
FAQs: Treatment and Answers
- Where can I seek treatment for my faecal incontinence?
- Will I need surgery to treat my faecal incontinence and will this result in a cure?
- If I have a complex sphincter injury which surgical treatment option is best, artificial bowel sphincter or the neosphincter?
- Can my faecal incontinence benefit from sacral nerve stimulation?
- Is a colostomy reversible?
- Patient follow-up
What is faecal incontinence and what are the causes?
The term incontinence means different things to different people and definitions vary even in medical literature. The World Health Organisation (WHO) defines continence as: the ability to voluntarily control defecation or stool expulsion, maintain this control even during sleep, distinguish between stool and gas and to defer defecation to a socially acceptable time. Given the above, it therefore holds that in simple terms, faecal incontinence is the inability to achieve continence. It is noteworthy that the concept of faecal continence remains a co-ordinated and complex interaction of various physiological processes that include: consistency of stool, compliance or distension of the rectum to receive increased quantity of stool, a local reflex mechanism, normal anal canal sensation with normal functioning of the internal and external anal muscle sphincter mechanism.
There are numerous causes of faecal incontinence, but by far the most common, is injury sustained by the anal muscle complex during the process of child birth. This is known as obstetric injury. Other causes include trauma or accidental injury during surgery to the anal area, while drugs, neurological disorders, congenital malformation, and colorectal diseases are less frequent causes.
Common symptoms
Most people suffering from incontinence will describe either one or a combination of the following three symptoms in varying degrees:
- Faecal Urgency: Patients experience the urge to expel stool but unfortunately just cannot get to the bathroom quick enough and as a consequence suffer an accident. This form of incontinence is due to weakness or injury to the external anal sphincter muscle complex.
- Passive Incontinence: In this form of incontinence patients have no urge or need to use the bathroom but are alerted to the fact that they have suffered an accident by the smell of stool. This symptom arises as a result of injury or dysfunction of the internal anal sphincter muscle.
- Post-defecatory Soiling: In this case patients are ordinarily continent but following stool expulsion, there is a near constant feeling that they have not fully emptied their bowels, associated with soling of their underwear and a frequent need to return to the bathroom. This type of incontinence is caused by obstruction to the normal flow of stool to the outside, either due to abnormal anatomy, that may be correctable surgically, or due to weakness or dysfunction of the pelvic floor muscle complex.
Diagnosing the condition
Primary Care
Your family doctor will want to ask you questions about your medical history and this is usually sufficient to define which of the above types of incontinence you may be suffering from. Unfortunately, obtaining an accurate history is an up-hill task for many family doctors because a lot of patients are not forthright with answers when questioned and, above all, are particularly embarrassed by the subject. However, perseverance on the part of the doctor often yields dividends and may even determine a possible cause of the incontinence if an intimate examination is permitted by the patient. Other tools available to the primary care physician include assessment of cognitive function issued by NICE (National Institute of Clinical Excellence) and an objective incontinence score using either the Cleveland Clinic or St. Mark’s incontinence questionnaire.
Secondary / Tertiary Care
In units specialising in the management of faecal incontinence, further clinical assessment is geared towards establishing the type, severity and cause of faecal incontinence before treatment is offered.
Further investigations in these centres may take the form of:
- Sigmoidoscopy / Endoscopy: In the outpatient setting, a small telescope is used to examine the rectum (sigmoidoscope) or alternatively, where necessary, a full examination of the whole colon using a fibre-optic camera (colonoscopy) is undertaken to exclude large bowel disease.
- Anorectal Physiology: This simply gives an objective measure of the existing function of the anal canal sphincter muscle complex and the rectum.
- Endo-anal Ultrasound: The ultrasound probe allows insertion into the anal canal and gives accurate images of the anal canal muscle complex so that injury or abnormal anatomy is identifiable and may be amenable to surgical correction.
- MR defecating proctogram: This highly specialised test virtually records the different processes involved in defecation so that any abnormal function or anatomical structure is defined and documented.
- Incontinence Score Questionnaire: These questionnaires objectively measure the type and severity of incontinence suffered by the patient. They are also especially useful in monitoring response or otherwise to treatment interventions.
Treatment and recent advances
Conservative Measures
Simple measures such as dietary modification and use of loperamide (such as Imodium) which are constipating agents helping to firm up stool and thereby minimise episodes of incontinence in cases associated with loose stool or diarrhoea. Some patients find that regular enemas assist in keeping the rectum empty while sanitary pads and occlusive plugs are equally effective in achieving reasonable levels of continence.
Biofeedback therapy and pelvic floor exercises are now firmly established first-line treatment strategies that must have been found not to have been of any benefit to patients before considering other invasive measures.
Sphincter Repair
Patients with disruption or deficiency of the anal muscle ring, due to childbirth or trauma, may be suitable for corrective surgery. The aim of the operation is to restore the anal sphincter muscle ring with specially placed sutures, this is known as an ‘overlapping sphincter repair’.
Antegrade Continence Enemas
This method of cleansing the entire large bowel with a litre or two of normal saline, involves surgically creating an access to the right side of the colon often utilising the appendix to fashion a ‘one way’ valve. More recently, special devices known as ‘caecostomy buttons’ have been found to be equally effective in washing out stool from the bowel and providing continence for periods of up to 48 hours in some cases. Cleansing the bowel via a rectal tube is known as a retrograde continence enema or irrigation and can achieve similar results to the antegrade approach, but there is evidence that the latter is faster and more efficient1. Furthermore, it has been shown that manipulating the fluid used for bowel cleansing can add to the efficacy of the antegrade method2.
Sphincter Implants / Drugs
In those patients with passive faecal incontinence as a result of disease or pre-mature wear and tear, improved continence has been reported by bulking up the muscle through direct injection with silicone bio-materials3. More recently, a similar strategy has been adopted for urge incontinence (Faecal Urgency). Drug agents whose actions include an increase in muscle tone have been used with some success to treat passive faecal incontinence.
Sacral Nerve Stimulation
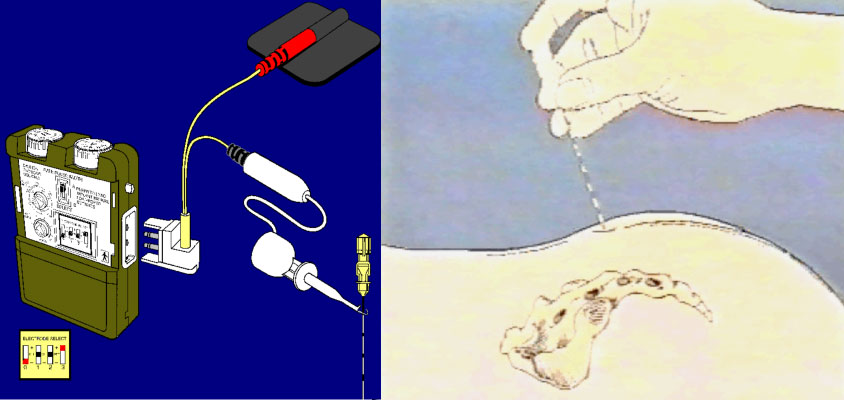
One of the more exciting recent advances in the management of faecal incontinence is sacral nerve stimulation. By direct electrical stimulation of the sacral nerve roots S2/S3, faecal continence is achieved in 50-100% of those previously incontinent. There is a preliminary stage using a temporary stimulator that should demonstrate at least a 50% improvement in incontinence, exhibited through the patient keeping a diary of their bowel movements, before implantation of the permanent device (Figure 1). The exact mechanism of action of this novel approach is unclear but it is believed to be due to neuromodulation of the process of faecal continence.
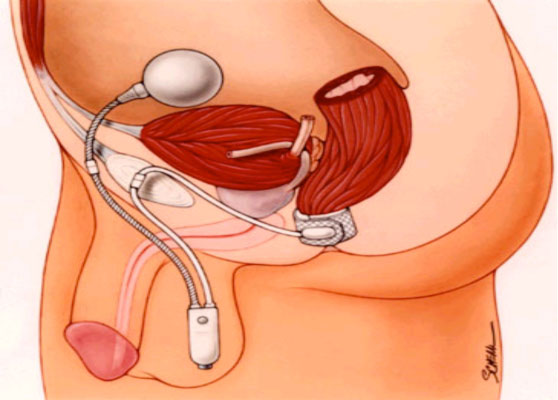
In the case of more complex sphincter injury, the artificial bowel sphincter (a modification of the artificial urinary sphincter) has been adapted to treat faecal incontinence. It consists of three components: a cuff around the rectum, a pump implanted in the scrotum or labia and a balloon sited in the lower abdominal wall (Figure 2). This device facilitates fluid transmission to the cuff to close the rectum (continence) and removal of fluid from the cuff, permitting expulsion of stool. Reported continence rates to liquid and formed stool using this device vary between 50–70%4. However, the potentially high complication rates of the artificial bowel sphincter indicate that patients should only be managed in highly specialised centres.
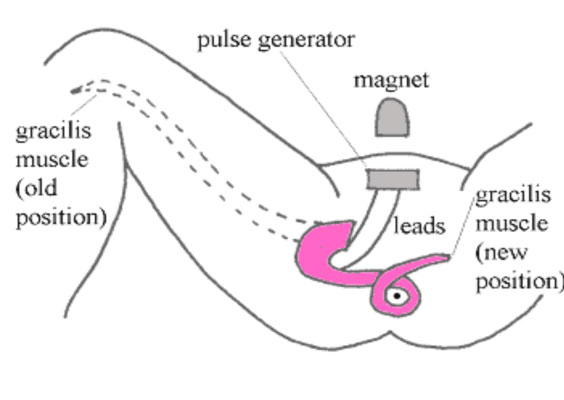
Muscle that is in close proximity to the anus can be mobilised and wrapped around the rectum or anal canal to create a muscle valve known as a neosphincter. The muscle wrap can be electrically stimulated to achieve continence through sustained contraction or allow stool expulsion by breaking the electrical circuit resulting in muscle relaxation (dynamic neosphincter). The thigh muscle known as the gracilis is most commonly used to fashion a neosphincter (Figure 3) but complications are frequent and, like the artificial bowel sphincter, should only be offered in specialised units. More recently, another form of neosphincter (physiological) has been described where it may be possible to control defecation voluntarily (without electrical stimulation) by joining the pudendal nerve to the nerve supplying the neosphincter. With more than 20 published cases in the literature, this approach holds promise for restoring normal continence in cases of faecal incontinence from complex sphincter injury.
The fashioning of a colostomy has been around for over 200 hundred years and may be considered in patients with faecal incontinence when all else fails. Contrary to general belief, most people with a colostomy live fruitful lives especially given the freedom offered by modern stoma appliances that allow them to engage in virtually all activities of normal daily living.
FAQs: Treatment and Answers
Where can I seek treatment for my faecal incontinence?
Your GP can refer you to the nearest specialist centre managing this condition.
Will I need surgery to treat my faecal incontinence and will this result in a cure?
Most patients do not require an operation and this is only considered as a last resort when all other conservative measures have failed. The benefits of surgery are immediate in those who undergo sphincter repair, but this benefit may be lost after several years. Further repair is possible however, with satisfactory outcomes.
If I have a complex sphincter injury which surgical treatment option is best, artificial bowel sphincter or the neosphincter?
Both treatments are equivalent in terms of restoring continence but the best strategy is to tailor treatment based on each individual patient’s personal circumstances.
Can my faecal incontinence benefit from sacral nerve stimulation?
With the exception of some patients with known severe neurological disorders, many people benefit from sacral nerve stimulation because the temporary stimulator predicts those most likely to benefit from implantation of a permanent device. This approach has led many clinicians to propose that it should be considered the first-line invasive treatment after failure of conservative measures.
Is a colostomy reversible?
This will depend on the reasons as to why one is having a colostomy. It can be designed by the surgeon to be a permanent or temporary solution although in most cases where every other measure has been tried without success, a permanent stoma (hole in the gut) should be considered.
Patient follow-up
Some patients are seen routinely in surgical outpatients to monitor their progress but the frequency of appointments will depend on the type of treatment undertaken and indeed, the personal circumstances of each individual patient. It is fair comment that most patients, following treatment for faecal incontinence, are not seen routinely by their doctors unless they develop some of the complications of treatment or if their symptoms return.
References
- Obichere A, Sibbons P, Dore C, Green C, Phillips RKS. Experimental study of faecal continence and colostomy irrigation. British Journal of Surgery 2000;87:902-908.
- Obichere A, Green C, Phillips RKS. Randomised cross-over trial of isotonic polyethylene glycol electrolyte solution and water for colostomy irrigation. Diseases of Colon & Rectum 2004;47:1506-9.
- Soerenson MM, Lundby L, Buntzen S, Laurberg S. Intersphincteric injected silicone biomaterial implants: a treatment for faecal incontinence. Colorectal Dis. 2009,11;73-76.
- Wong D, Congilosi SM, Spencer MP et al. The safety and efficacy of artificial bowel sphincter for fecal incontinence: results from a multicenter cohort study. Dis Colon Rectum 2002;45:1139-53.
For further information on the author of this article, Consultant Laparoscopic and Colorectal Surgeon, Mr Austin Obichere, please click here.
Associated with the nervous system and the brain.
Full medical glossary

