Knee pain can be a debilitating condition and in many cases patients may feel that surgery is their only option. This article explains the different types of knee complaints and how they can be treated using non-invasive and non-surgical techniques.
Contents
- Introduction
- Knee Osteoarthritis
- Meniscal tear
- Anterior cruciate ligament rupture
- Anterior knee pain
- Mechanics of knee complaints
- AposTherapy
The objective of this article is to introduce different knee injuries and conditions, what they actually are, and how AposTherapy, a novel non-surgical treatment modality can address the underlying causes of these knee conditions. Being a Chartered Physiotherapist with experience of working for a professional football club and for the past three years with AposTherapy, knee conditions are my main interest and area of expertise. I am fortunate to work closely with like-minded professionals who have fantastic clinical skills whilst at the same time being able to develop strong links with fellow healthcare professionals throughout the capital, some of the best in the world. We all strive to provide the best solution for our patients, whatever the knee complaint may be.
Introduction
The knee is the largest joint in the body. It is shaped like a hinge joint, which means that it has two main directions of movement: bending the knee (flexion) and straightening the knee (extension). There is some element of rotation in the movements of the knee as well, allowing us to turn our toes inwards or outwards. The knee endures repetitive and relatively large forces throughout our lives since it bears the weight of the body in any activity we perform while being on our feet. Within the knee joint there are three joint surfaces: the Medial and Lateral Tibio-Femoral joint surfaces and the Patello-Femoral joint surfaces. The bones are held together with a web of ligaments and a fibrous capsule. The movements of the knee are generated by the brain via nervous impulses that activate the many muscles that act upon the knee to provide controlled movement of the joint whilst maintaining stability and balance. This process is called neuro-muscular control; effective neuro-muscular control is vital to provide stability and is the basis for all normal healthy movement and activity.
Knee pain is common, we are all likely to experience it at some point during our life, and of course it depends on its severity and our functional demands as to whether we choose to do something about it. This article will focus on four common knee conditions, however the principles of treatment that will be introduced can be applied to other knee conditions as well.
Knee Osteoarthritis
Osteoarthritis (OA) was originally defined as the chronic degeneration of the joint surfaces. It can affect any or all of the three knee compartments. OA is primarily a biomechanical condition that affects the older population but can result from traumatic injuries in younger individuals. Common symptoms include joint pain, primarily during weight-bearing activities, stiffness following periods of rest, swelling, and a reduction in joint range of motion. In the past two decades there has been a growing understanding in medicine that, alongside the wearing away of the cartilage, the muscles around the joint can also begin to alter the way they work in an inefficient way. This inappropriate activity of the muscles, called bracing, increases the loads acting on the injured joint, decreases the joint’s range of motion and is considered to be a detrimental factor in the initiation, progression and worsening of OA.
Meniscal tear
There are two crescent-shaped menisci in the knee joint, one in the medial and one in the lateral knee compartment. A meniscus is a combination of fibrous material and cartilage. The function of the menisci is to maintain a space between the thigh bone and the shin bone, distribute the loads through the knee joint and help maintain joint stability during movement. Both the symptoms and the treatment required depend greatly on the size of the tear. In young people, a meniscal tear can result from a traumatic injury where it may cause the joint to ‘lock up’. In older people it is usually a result of joint degeneration and is therefore common in patients with OA. A large tear causing the knee to lock may be extremely painful and in most cases requires surgical intervention. A smaller degenerative tear may be very painful but symptoms should gradually reduce and surgery is not recommended in this instance. It is important to note that some of the tears in young people can be small and therefore do not necessarily demand surgical intervention.
Anterior cruciate ligament rupture
The anterior cruciate ligament (ACL) is one of the largest ligaments in the body and is located deep inside the knee joint. It has two main functions: it acts as a joint stabiliser by connecting the two bones of the knee and preventing the thigh bone from moving too far forward on top of the shin bone. It also plays a very important role in telling the brain what position the knee joint is in and whether or not it's moving. This is because it contains a very high number of sensors (nerve fibres). It usually takes a huge force to rupture the ACL, therefore it is usually a sports injury. The symptoms include an audible ‘pop’ at the time of injury followed by immediate swelling. Pain afterwards is not usually severe, however a feeling of instability can be very unnerving and uncomfortable, particularly on activities such as descending stairs or changing directions. In some cases surgery is required where a graft is used to act as the ligament, however, whether surgery is undertaken or not, the key to success is a dedicated rehabilitation programme. This is because the body, and indeed the brain, need to learn to receive the information regarding the knees’ movements from structures, other than the torn ACL, in and around the knee. The graft used in the surgery does not contain the necessary nerve fibres to supply that information. That may be, in part, the reason why recent studies have shown that the result of an ACL reconstruction followed by rehabilitation is in the vast majority of the cases identical to the result of rehabilitation without the surgery. The conclusion is that in most cases, rehabilitation is the crucial ingredient in returning to activity following an ACL rupture.
Anterior knee pain
This is an umbrella term that covers conditions that affect the patella. The underside of the patella has a layer of cartilage which can be damaged if the muscles that control the patella are not functioning correctly. In a younger person this joint surface irritation whereby the cartilage is thinned or softened is often referred to as chondromalacia patella, meaning simply, damage to the cartilage of the patella. When the cartilage is very degenerated the condition may be termed Patello-Femoral Joint Arthritis. In many cases of anterior knee pain however, there are no obvious changes to the cartilage and the term given to this group of symptoms is patellofemoral pain syndrome (PFPS). The symptoms in all cases are similar including pain while on stairs. Exercise can induce a flare up of symptoms lasting a few days and finally ‘cinema-goers knee’ can occur, pain that is felt during long periods of sitting with the knee bent. Treating these conditions traditionally involves focusing on re-educating the muscles around the patella to improve the tracking or movement of it during activities. Self-management of activities and lifestyle is also vitally important with these conditions.
Mechanics of knee complaints

There are several factors pertaining to all these pathologies which should be considered when discussing the best course of action. These factors include pain, biomechanics and the body’s own neuromuscular control. For each pathology, and for each person, these factors interplay in a slightly different manner. That is why each patient must be individually assessed and the solution for one patient may not be the best solution for another.
Pain
Pain is an unpleasant sensation caused by a stimulus which either damages the tissues of the body or poses a potential danger to the integrity of the body. Pain is sensed by special receptors connected to specialised nerve cells which transfer the stimulus to the brain. Once the brain "deciphers" the message from these nerves, pain is felt. The pain receptors and nerves, which make up a specialised nervous system dedicated to pain, are situated throughout the body. The level and duration of pain we feel can vary depending on what has caused it. For example, an acute ligament injury may cause severe pain for a relatively short time, a chronic condition such as OA may cause pain with every footstep, whilst an overuse injury may only cause low level pain during the activity. Everybody’s pain is different and in most cases will vary depending on many factors.
Healthcare professionals aim to reduce pain as quickly as possible. We can use a number of ways to do this, from ice packs, to supports and braces, to medications, all with varied success; often pain relief can be achieved at rest but is very difficult to maintain during movement. The success is often determined by what is causing the pain in the first place. In some of these knee conditions the pain is caused by a mechanical fault in the joint (uneven load distribution, lack of smooth gliding between the bones etc.) in which case medications such as anti-inflammatory drugs will be of little use. In other cases the pain is caused by an increased sensitivity of the nerves in the pain system, leading to an amplification of any small stimulus arising from the knee. In these cases, analgesic medication along with graded activity should be advised.
In any activity we perform while bearing weight on our feet there are forces and loads which the joints in the leg have to cope with. These loads are caused not only by the weight of the body but also from forces which, for the sake of simplicity, are called recoil forces from the floor. You can feel them if you concentrate on the feeling in your leg when your foot makes first contact with the ground during a brisk walk. This recoil force, called the ground reaction force (GRF) alters as we move and its effect on the knee depends on the activity and the position of the knee. When a knee is misaligned, as it is in people who are bow-legged for example, the force acting on the knee during activity is altered. In these cases there is a much greater load born on the inner part of the knee than is normal. This may hasten the process of degeneration of the medial (inner) part of the knee. A lot of people who have OA have bowed knees, which means that they have greater load on the damaged part of the knee. As the joint degenerates further it often becomes more bowed, thus further increasing the load on the damaged part of the joint. This is why, when considering the solution for various knee problems, the alignment of the knee, and of the entire leg must be taken into account since it has a direct bearing on the loads affecting the knee joint and is therefore directly connected with the pain and difficulty in function that that person feels as well as determining the rate of progression of the knee conditions.
Neuro-muscular system
There is another vitally important reason why we must reduce pain, which relates to the system that provides us with the ability to move in the first place: the neuro-muscular system.
As discussed, normal muscle activity is crucial to maintaining healthy joints. Normal muscle activity is when a muscle contracts or elongates in a controlled manner with the appropriate force to provide a co-ordinated movement. Pain causes abnormal muscular activity! It causes certain muscles to work continuously to try to protect the damaged area, which is known as bracing. When this occurs other muscles will not work hard enough and effectively become ‘lazy’. If the injury heals quickly the bracing will reduce gradually and the muscles will return to co-ordinated activity ensuring the joint moves smoothly. But in chronic injuries, such as mentioned above, the muscles are working incorrectly for too long. They become very tight and painful, they cannot provide sufficient stability for the joint and they do not produce co-ordinated ‘normal’ movement. In other words, they become a part of the problem. To the same extent a muscle that has become ‘lazy’ due to pain will be ineffective at providing stability and may not function properly to provide normal movement. So pain, as well as being unpleasant, has a very detrimental effect on allowing us to recover and function normally.
There are examples from daily life we all experience at some point or another which illustrate this mechanism. The stiffness felt in the lower back in the days following an acute back pain is mainly due to bracing muscles. If an athlete twisted his knee badly during a football match and tore his ACL, he will find straightening the knee impossible due to bracing of the hamstrings. These are both examples for acute injuries. In chronic long-standing conditions, abnormal movement patterns will be present for a long time. These abnormal movement patterns tend to both deteriorate and expand over time. It makes sense how with time, the individual’s ability to function normally reduces; previously mundane or easy tasks become harder or more tiring simply because the muscular control is abnormal. This is why clinical research shows that an individual who suffers an ACL rupture will develop OA changes within 15–20 years, irrespective of whether they have had surgery to repair the ligament or not. This is also why people who have had a meniscal tear are at risk of developing OA. Treating all knee conditions with traditional methods can be difficult but this proves why the ‘correct’ treatment, at the earliest stage possible is essential to protect the weight-bearing joints in later life and prevent chronic conditions.
Therefore the two fundamental components discussed in this article must be addressed in order to provide the optimal treatment. Firstly, reduce the pain. This can be achieved by redistributing the loads and forces acting on the knee. Once the pain is reduced and the load is properly distributed the issue of retraining correct neuro-muscular control has to be addressed. This will allow for normal movement and stability of the joint. These principles remain the same for the four main conditions affecting the knee.
AposTherapy
AposTherapy is a non-invasive, non-pharmaceutical treatment that has been specifically developed to encompass the key principles of treatment in an easy to use format. The treatment is based on a foot-worn biomechanical system that patients wear for up to an hour as part of their daily routine either at home or in the office. The unique therapeutic effects of the system are achieved with two convex pods, called Pertupods (pods which provide perturbation), attached to specially designed footwear under the main weight-bearing areas: the heel and forefoot. An AposTherapist, a specially-trained chartered physiotherapist, adjusts the Pertupods by selecting their location on the sole of the shoe, as well as adapting their height, convexity level and resilience based on the patient’s specific condition. The treatment is innovative and ground-breaking because it unites all the principles discussed above.

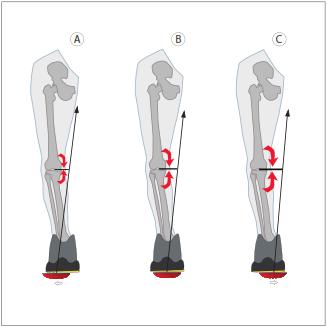

AposTherapy offers a unique way to address the first component of pain. By altering the position of the two Pertupods, the AposTherapist is able to adjust the way the foot makes contact with the floor, thus altering and redistributing the loads in the knee. The infinite adjustments that an AposTherapist can make to the system means that within a very short space of time pain can be reduced significantly as the therapist shifts forces away, or off-loads damaged areas. Importantly, the benefit of this can be felt almost instantaneously during the first treatment session. This can be applied to all knee conditions, whether it is a joint surface problem that needs off-loading or a ligament injury that needs supporting. By addressing both the load distribution and providing the necessary pain reduction we are providing the perfect platform to address the second component: rehabilitation of neuro-muscular system.
To achieve an effective rehabilitation of neuro-muscular control, the rehabilitation programme has to be functional, repetitive and done subconsciously. AposTherapy stands at the forefront of functional rehabilitation as it combines these three principles very simply and effectively.
Functional
If a person wants to learn to ride a bike it will be rather pointless if he trained only in jogging. This is because our neuro-muscular system learns each activity separately. So the fact that a person is a good runner will not necessarily mean he knows how to ride a bike. As previously discussed, most knee conditions are symptomatic of everyday functional activities which directly imply that rehabilitation needs to take place in all of the activities which cause pain e.g. walking, climbing stairs, sitting etc.
Repetitive
Each time a person performs an activity, be it bouncing a ball or playing the piano, the nerve cells in the brain and spinal cord must communicate with each other in order to issue the correct commands for the muscles carrying out this activity. When the activity is unfamiliar or has been carried out incorrectly beforehand, the nervous system must form new connections between the nerve cells and the relevant muscles. It therefore follows that the aim of any neuromuscular rehabilitation is to create changes in the structure and function of the nervous system. In order to create such a process the activity must be repeated many times. Clinical research shows it takes between 10,000–15,000 repetitions in order to establish a desirable movement pattern; in other words, practice makes perfect. While walking with the AposTherapy foot-worn biomechanical system every single step is a repetition of the corrected movement patterns thereby enabling tens of thousands of simple repetitions over a short period of time. Once the desired movement pattern is instilled, the body performs this pattern even without wearing the biomechanical system.
Subconscious
In order to make a certain movement pattern subconscious, we need to learn it in a subconscious way. Consciously learning a movement pattern takes a lot of concentration, can be very difficult and tiring, and has been shown to be less effective than when the movement is performed subconsciously.
AposTherapy uses the convexity of the Pertupods to provide a controllable level of instability to the system. On a neuro-muscular level it stimulates the ‘lazy’ muscles to wake up, and at the same time the braced muscles have to relax and respond to the changes in the joint. By wearing the system to go about your daily routine, AposTherapy utilises all the functional activities that we do in our lives. From standing up from a chair to loading the dishwasher, the patient remains comfortable as the damaged area is off-loaded. The neuro-muscular system is being trained and stimulated to perform properly during normal everyday activity. Each step taken, or each movement made is a repetition. The number of repetitions required to retrain the stability and control around the joint now seems much more achievable as the system is worn every day for a short period. During this time the brain is re-learning normal patterns of motion and as the treatment continues these movement patterns are learned and assimilated into daily activities without the system. In AposTherapy we refer to this as 'carryover effect' and this is the main objective of treatment i.e. instilling corrected patterns of motion. AposTherapy reduces pain and teaches the body the correct way to function again, by doing so the benefits are felt throughout the whole day allowing the patient to return to activities that had previously become impossible.









