When you are in the unfortunate position of having been diagnosed with a knee condition that requires partial or total knee replacement surgery, the next step involves asking questions in order to ascertain the most appropriate knee procedure, and to find the best surgeon for you.
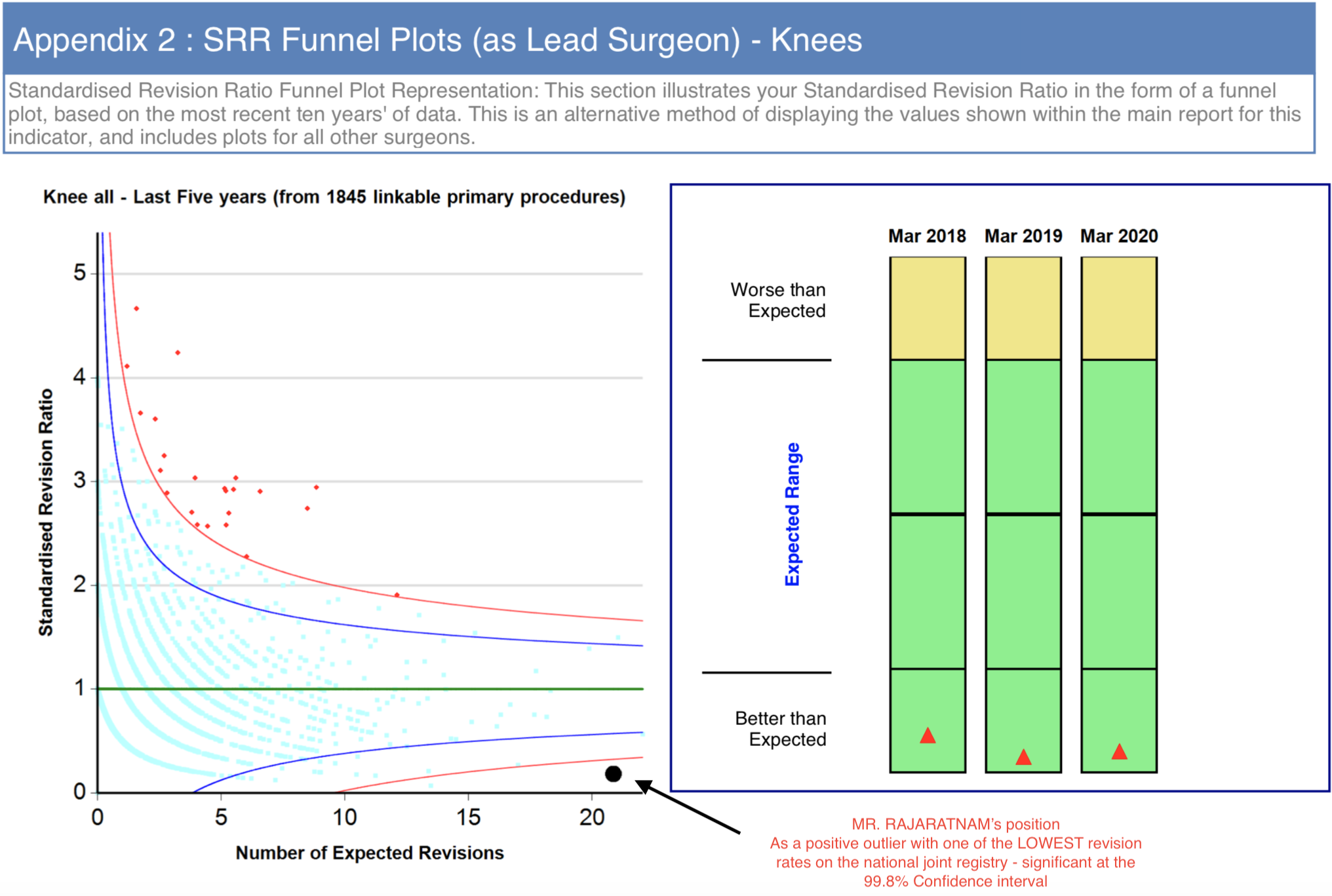
Choosing the best knee surgeon is no longer a matter of guess work, broad research and / or luck. Data is now collected and published on the performance of all surgeons, and their outcomes can be compared. According to the National Joint Registry, one of the top performing knee surgeons is Mr Sam Rajaratnam. Total Health have therefore asked Sam to explain the secret to getting excellent results in knee replacement surgery.
Here are his top ten answers:
1. What is meant by a good outcome in knee replacement surgery?
Patients have knee replacement surgery to alleviate pain, instability, and loss of function in their knee. A good outcome is where the patient’s quality of life is significantly improved after their joint replacement. From a surgical perspective, a good outcome is scientifically quantifiable. The UK National Joint Registry (NJR) collects data on every joint replacement that is done both in the National Health Service (NHS) and the private healthcare sector. This data can be individualised to the surgeon and the hospital.
2. How quickly will I be mobile again following surgery?
If your knee replacement is being performed by a surgeon who works in a joint replacement unit that believes in “rapid recovery” or “enhanced recovery”, you could expect to get up and be walking three to four hours after your surgery.
3. How can I check to see how good the surgeon and their team actually are?
There is increasing transparency in healthcare outcomes within medical practice in the UK. You could visit the NJR surgeon profile section and search for your surgeon or intended hospital to see how many joint replacements that surgeon / hospital performed in the preceding year.
 4. What do the NJR results actually mean to me?
4. What do the NJR results actually mean to me?
Having an idea of your surgeon’s experience, the volume of their practice each year, and their overall revision rate, will be very reassuring to you when you are choosing the correct person to perform your joint replacement.
5. How do surgeons get such good outcomes?
Mr Sam Rajaratnam suggests that improving surgical outcomes by “cumulative marginal gains” is key. This is where the addition of a number of small improvements cumulatively makes a big difference to the outcome of a surgical procedure. Specialising in just one part of the body helps tremendously, and having a settled multidisciplinaryteam working with you makes a big difference too. Ultimately, it is important to have an expert surgeon who has a sub speciality interest in knee replacement surgery, a dedicated and regular anaesthetist who has an interest in multimodal analgesia, expert nurse consultants and physiotherapists and excellent ward care in place during your joint replacement surgery.
 6. What are the new improvements that have been made in knee replacement design by the manufacturers over the last two decades?
6. What are the new improvements that have been made in knee replacement design by the manufacturers over the last two decades?
Implant manufacture has improved tremendously over the last couple of decades. In the opinion of Mr Rajaratnam, one of the biggest improvements was when the polyethylene lining (which mimics natural cartilage), started being manufactured in a vacuum, therefore substantially improving its material properties and its resistance to wear.
7. Are modern joint replacements really surface replacements?
To a certain extent the answer is probably, "yes". The surgeon removes a small amount of the exposed bone and cartilage and then tries to custom fit a surface that mimics the natural surface of the knee. The designs of knee replacements have now changed and adapted to accommodate a custom fit and a more natural feel, thereby allowing for better and a more natural function of the knee joint.
8. What are the improvements in soft tissue handling around knee replacement surgery?
A knee replacement operation can now be considered mainly as a soft tissue operation with some implants involved. Techniques have now developed to reduce the size of the incision around the knee replacement, to respect and preserve all of the normal soft tissue envelope, and to shape an implant to the new surface causing minimal damage to the surrounding tissue. This includes techniques to reduce the bleeding around the operation, and avoiding damage to attachments of tendons, muscles and ligaments around the margins of the joint .... see more
9. How long are knee replacements lasting?
With the before mentioned improvements in manufacturing, alignment and implantation, knee replacements are lasting a long time, often two or three decades.
10. How do you choose between a partial and a complete knee replacement?
A partial knee replacement is a slightly smaller operation, allowing a patient to recover a little bit faster in the short term, but does pose the possibility of the remainder of the damaged knee failing, and necessitating further revision surgery and additional procedures subsequent to the first procedure. A full surface replacement is slightly more invasive, but does address the remainder of the joint at the first sitting. To get the balance right between the two, a careful analysis of the joint needs to be undertaken pre-operatively by your surgeon.
Mr Sam Rajaratnam says, "Ultimately 'getting it right the first time' is the best chance to achieve a happy patient and satisfactory results, and careful pre-operative decision making is essential. He goes on to say, "Most of my patients will return to sailing, cycling, rambling, tennis, skiing and golf very happily".
See also:
Who are the best knee surgeons in London?









