Groin Injuries
A groin tear can be hugely painful and there is often confusion caused by the varying medical terminology. A groin tear syndrome is often referred to as Gilmore's Groin, however, the names or diagnostic terminology may also include the following types of terms:
-
Groin disruption
-
Inguinal disruption
-
Sportsman's hernia
-
Inguinal related groin pain
Diagnosing and Treating Gilmoire's Groin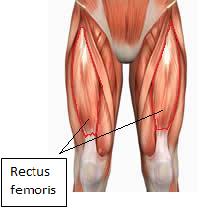
These types of groin injury are nearly always sports related, either as a result of insufficient warm up, from pushing the body too hard, incorrectly positioned kicking feet or as a result of a collision. However, the injury can happen at any time to even the most elite athletes. When it happens it can be utterly debilitating and you will need to see a doctor.
To begin with your doctor will take your medical history, which involves working out what happened and your symptoms. You will also be asked about your general health and any operations or illnesses you may have had as well as about medications you take or allergies to any medicines. You will then need an examination in order to establish precisely which types of movements cause the pain.
In approximately a third of people there is a highly specific injury that brings on the pain. There are a number of typical activities leading to the causes for this type of pain. These activities can include the following:
-
over stretching,
-
excessive kicking
-
miskicking
-
the leg being forced away from the body or turned outwards forcibly.
If the injury has come about as a result of “overuse” or a poor tecnique, the symptoms usually come on gradually. In these cases, and especially when playing sport increased pain in the groin will often be felt in situations involving:
-
sudden acceleration,
-
sprinting,
-
twisting and turning,
-
lunging,
-
dead ball kicking or
-
long ball kicking.
In many cases, sporting people complain that their groin is stiff and sore for several days after exercise and there may be pain in specific situations such as:
-
with sit-ups,
-
rising from a low position (for example getting out of bed or in and out of a car),
-
coughing,
-
sneezing and
-
any sudden movement.
The difficulty for most people trying to work out what is happenng is that there is often nothing to see in the painful groin and in particular there is no lump. In the case of a sudden, severe, tear there may be considerable bruising, but this is rare.
Groin Examination
When examined via the scrotum, the superficial inguinal ring is dilated and tender and there is a cough impulse indicating a groin disruption
A groin examination is initially performed standing up and then lying down. The purpose of this is to look at the site of the pain. The movement of your hips will be checked to establish any particular movements that cause pain. When the groin itself is examined the key is the feel the “superficial inguinal ring”. In men this can be felt by (gently!) pushing up inside the top of the scrotum towards the groin.
Why you may be asked to cough
When the groin is torn this ring (which normally contains the cord bringing all the tubes and blood vessels to the testicle) gets pulled apart (dilated) and it is possible to feel the back of the groin (called the inguinal canal) through it. When the groin is torn this will be painful (compared with the uninjured side) and coughing will make the damaged groin muscles bulge forward. The findings are usually written as “when examined via the scrotum, the superficial inguinal ring is dilated and tender and there is a cough impulse indicating a groin disruption”. In women, for obvious reasons, the examination of this area is less helpful.
Differentiating a Groin Tear from other Conditions
The trouble is that there are many other medical conditions such as arthritis and muscular tears that produce similar symptoms to a Gilmore's Groin. Each condition requires a completely different type of treatment or approach and so it is essential to get an accurate diagnosis.
The combination of medical history, physical examination and the MRI scan can make the correct diagnosis most of the time, the trouble is that this approach alone is not always totally sufficient. There are lots of other conditions that can cause similar symptoms and signs and it can sometimes be difficult to work out exactly what is causing the pain.
The other types of conditions that can cause similar, or sometimes identical, pains include:
-
fractures,
-
inflammation of the pubic tubercle (“osteitis pubis”),
-
arthritis,
-
bursitis,
-
muscular tears in the adductor or
-
thigh muscles and the
-
syndrome of femoro-acetabular impingement.
In the case of a femero-acetabular impingement the “ball” of the hip joint on the top of the thigh bone, is the wrong shape and this can cause tears around the joint itself as well as inflammation. This can sometimes cause exactly the same pains as a groin tear. Whilst the abnormal shape of the hips is easily seen on the MRI scan, in many people this does not seem to cause any problems and it needs no treatment.
It is therefore important that a diagnostic radiologist who specialises in the groin is responsible for reporting on the imaging scans.
Specialist Groin Musculoskeletal Radiologist
The next stage is to arrange any investigations to help confirm the diagnosis. The best single investigation now is a high resolution (3T) MRI scan. Not only is the high resolution important but it is also vital that the “correct protocols” are carried out. This means that the scans are done of the correct areas with the right resolution to see all the muscles and the hip joints. In addition the scans must be looked at (“reported”) by a specialist musculoskeletal radiologist who is used to working in a specialist groin team. Scans that do not meet these requirements may be inadequate and a further scan may need to be done. Occasionally an ultrasound scan may also be helpful as may x-rays of the hips and pelvis, or a test called a bone scan, but it is the MRI that is most important.
Surgical Repair of the Groin
If, following discussion of your results, you wish to have your groin surgically repaired you will be given written information about the condition of Gilmore’s Groin, the operation and how it is done, how to look after your wound after the operation when you are at home and some rehabilitation exercises to start a few days after the operation. In addition you will be given the clinic telephone contact numbers if you need any further advice. Everyone is seen after 4 weeks to check that everything has healed up and that the rehabilitation is progressing as it should. Most people are discharged at this stage, but some may need a further check in a few more weeks.
Inflammation of one or more joints of the body.
Full medical glossary
A fluid that transports oxygen and other substances through the body, made up of blood cells suspended in a liquid.
Full medical glossary
An imaging test that uses radioactive substances to evaluate the whole musculoskeletal system.
Full medical glossary
Inflammation of one or more of the small sacs of synovial fluid (bursae) under the skin, normally found over joints and between tendons and bones. They act as cushions between two surfaces that may rub against each other.
Full medical glossary
A sign that a doctor looks for when examining a swelling, especially a hernia. A positive cough impulse means that the swelling expands when the patient coughs.
Full medical glossary
The process of determining which condition a patient may have.
Full medical glossary
The basic unit of genetic material carried on chromosomes.
Full medical glossary
When part of an organ pushes through the wall of the body cavity that normally holds it. Hernias can develop in many different parts of the body.
Full medical glossary
The body’s response to injury.
Full medical glossary
Relating to the area around the groin.
Full medical glossary
An abbreviation for magnetic resonance imaging, a technique for imaging the body that uses electromagnetic waves and a strong magnetic field.
Full medical glossary
Tissue made up of cells that can contract to bring about movement.
Full medical glossary
Relating to the skeleton and its attached muscles, cartilage, tendons and ligaments that gives structure to the body and enables movement
Full medical glossary
Inflammation of bone, most commonly caused by infection.
Full medical glossary
The bony basin formed by the hip bones and the lower vertebrae of the spine; also refers to the lower part of the abdomen.
Full medical glossary
A craving to eat non-food substances such as earth or coal.
Full medical glossary
A pale yellow or green,creamy fluid found at the site of bacterial infection.
Full medical glossary
A doctor specializing in the interpretation of imaging techniques for the diagnosis and assessment of disease.
Full medical glossary
The treatment of a person with an illness or disability to improve their function and health.
Full medical glossary
The sac that contains the testes.
Full medical glossary
One of two male sex organs, also calles testes, that produce sperm and the hormone testosterone.
Full medical glossary
A diagnostic method in which very high frequency sound waves are passed into the body and the reflective echoes analysed to build a picture of the internal organs – or of the foetus in the uterus.
Full medical glossary












