There have, for about 30 years, been a few women's health specialists like Professor John Studd and Rosie Greenblatt who gave testosterone to women for various psycho sexual and mood problems. This article explains why women need testosterone and how they can get help.
Contents
- Introduction
- Normal testosterone levels in women
- Differentiate the hormone deficiency
- The five symptoms of female androgen deficiency syndrome (FADS)
- Symptoms of androgen deficiency havve profound effect
- Evidence-based hormone therapy
- Who should be treated with testosterone?
- Dangerous nymphomania
- Most Vile and Obscene Picture
Introduction
Early testosterone was given to women in the form of implants as that was the only preparation licensed for use in women. There are now gels licensed for men which can be used off-licence in a smaller dose for women and at last, a testosterone patch has recently received a licence for use in women who have had a hysterectomy and bilateral salpingo oophorectomy.
There is often a delusion amongst patients that testosterone is a male hormone. Of course it is a normal female hormone but it is not always understood that in healthy young women it is present in 10 times the level as oestradiol. Similarly there are many more Androgen receptor sites in the female brain than oestrogen receptors. Androgen levels begin to decline at the age of 20 and by the time of the natural menopause the levels are much reduced. Everyone is aware that oestrogen levels fall with the menopause but there is also a 50% fall of testosterone after a natural menopausal and a 75% fall in testosterone after bilateral oophorectomy.
Normal Testosterone levels in women
Healthy young women produce about 100μg-200μg of testosterone each day which is about 5% of the daily testosterone production in men. Half of this is derived from the ovaries and half from the adrenal glands as the hormone DHEA is converted to testosterone in the body fat. The decline in androgen levels contribute to a decline in sexual desire, arousal and orgasm and also has effects on general well-being, energy, mood, bone physiology and decreased muscle mass as well as hot flushes.
Differentiate the hormone deficiency
Healthy young women produce about 100μg-200μg of testosterone each day which is about 5% of the daily testosterone production in men. Half of this is derived from the ovaries and half from the adrenal glands as the hormone DHEA is converted to testosterone in the body fat. The decline in androgen levels contribute to a decline in sexual desire, arousal and orgasm and also has effects on general well-being, energy, mood, bone physiology and decreased muscle mass as well as hot flushes.
It is important to differentiate the symptoms of oestrogen deficiency in post-menopausal women from testosterone deficiency. The oestrogen deficient woman has typical climacteric symptoms of hot flushes, sweats, sleep disturbance, mood changes and vaginal dryness. These symptoms do, of course, overlap with many of the symptoms of testosterone deficiency known as the Female Androgen Deficiency Syndrome (FADS).
The Five Symptoms of Female Androgen Deficiency Syndrome (FADS)
There are typically five symptoms of this condition:
- Decreased well-being and self-confidence.
- Decreased energy.
- Decreased sexual desire and arousal.
- Increased depression.
- Headaches.
Symptoms of androgen deficiency have profound effect
As gynaecologists we commonly see this symptom complex of androgen deficiency in women who have had a hysterectomy and bilateral oophorectomy and have been maintained on a low dose of oral oestrogens for several years. They have no hot flushes and sweats and have no vaginal dryness but they do not feel well. They have predictable problems with loss of energy, loss of sex drive, depression, headaches and loss of self-confidence. These symptoms which have a profound effect on quality of life respond well to the addition of small amounts of testosterone.
It is no surprise that FADS occurs commonly after bilateral salpingo-oophorectomy but we do not know its incidence after hysterectomy with ovarian conservation. It is not rare. Nor is it rare in intact post-menopausal women, peri-menopausal women, or even younger women who have problems of sexual response. The diagnosis should be made by taking a careful history of poor sexual response and other appropriate symptoms within a good relationship where these are also helped by a response to testosterone therapy. A pre-treatment testosterone level is not very valuable for the diagnosis as we usually measure total testosterone. Ninety five per cent of total testosterone is bound to sex hormone binding globulin (SHBG) and therefore, inactive. The free testosterone is more important for function but difficult and expensive to measure in these tiny quantities.
Evidence-based hormone therapy
An early uncontrolled study showed that oestrogens improved dyspareunia and vaginal dryness and libido in 80% of this group. The addition of testosterone improved libido in 12 out of the remaining 15 patients who had not responded to oestradiol. Subsequently there have been a few better randomised controlled studies showing the benefits of testosterone therapy and latterly, the effects of transdermal testosterone patch on sexual desire, sexual activity, orgasm, pleasure, responsiveness and self image with a corresponding decrease in sexual distress. The patch Intrinsa™ is recommended in a dose of 300μg and applied twice weekly.
The value of testosterone over oestrogen and placebo was shown in trials 20 years ago by Sherwin and Gelfand with implants of hormones after hysterectomy and bilateral salpingo oophorectomy. The clear result in this study was that the addition of testosterone improved sexuality, decreased depression and improved general health scores. We have reported a prospective study of 200 women having implants of oestradiol and testosterone after hysterectomy and oophorectomy showing the long term improvement over many years of libido orgasms depression anxiety and energy. In spite of this, the vast majority of women who have lost their ovaries at surgery are not offered testosterone for reasons which are very hard to understand.
Although there is a tendency to equate testosterone therapy with a sexual response with increased sexual episodes, libido and easier orgasms it is important to realise that there is a non-sexual component in these benefits. Women speak of greater self confidence, greater mental acuity, less depression and they even speak about greater efficiency and communication within their work. They are also aware of increased self worth and yet they behave like “wanted women rather than neglected ones”. These non-sexual components, although important, are more difficult to assess in trials and therefore, alas have not been done.
Who should be treated with testosterone?
This information does leave the question about who should be treated. Clearly, nearly all women who have had a bilateral oophorectomy should have appropriate hormone replacement therapy which should consist of oestradiol and testosterone. Now that testosterone is available on licence for women it is hard to justify oophorectomy in pre-menopausal women without replacement of testosterone. Although there is no licence for non-hysterectomised women to receive testosterone there is no doubt that good, well-experienced doctors will prescribe testosterone for the appropriate symptoms in women who have an intact uterus and ovaries, and even in those that are pre-menopausal with the appropriate symptoms. Prescribing “off-licence” is controversial but that does not mean that it should be forbidden.
Dangerous nymphomania
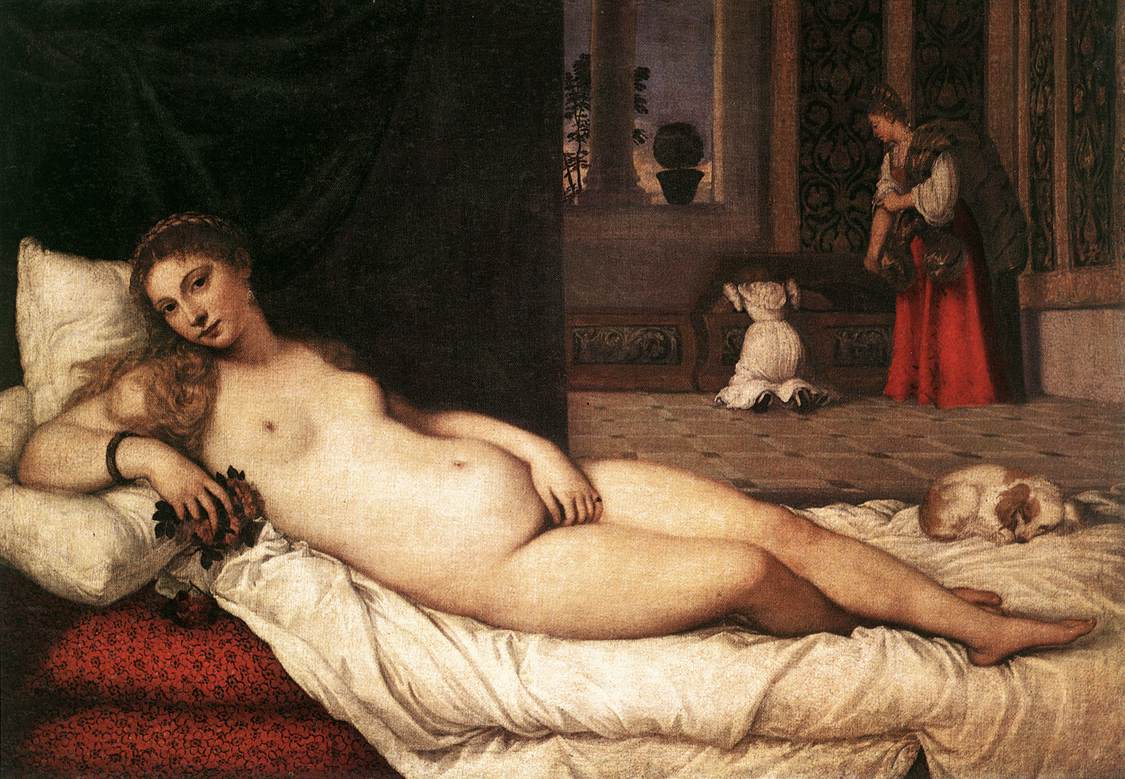
Historically, it is most interesting that whilst modern society and medicine are concerned that women should have a satisfying sex life, it was not always so. This is far removed from the attitudes in the last half of the 19th Century when nymphomania and masturbation were thought to be serious diseases which led to paralysis, coma and death. There were tens of thousands of women who underwent removal or irradiation of the clitoris to remove their sexual desires although in earlier centuries female sexuality was respected, as we can see from Titian’s Venus of Urbino in 1583.
Vilest and most Obscene Picture The World Possesses
It is clear from her interned fingers and the position of her left hand and the look on her beautiful face that the position is not a matter of modesty. She is clearly enjoying herself, probably teasing her lover, the Duke of Urbino. A famous, furious comment, on this picture was Titian’s Venus of Urbino in 1583 made by Mark Twain protesting that artists can paint but writers can not write about such sexual events. This can be obtained by “Googling” Venus, Titian and Mark Twain. It is worth a few minutes of your time.
However while enjoying the “foulest, the vilest, the obscenest picture the world possesses” remember that many of your female patients are deficient in testosterone and now with patches and gels it is easy and safe to administer.
There is no longer any excuse not to do so.
For further information on the author of this article, Consultant Gynaecologist, Professor John Studd, please click here.
This article first appeared in Capital Doctor.
The time of a woman’s life when her ovaries stop releasing an egg (ovum) on a monthly cycle, and her periods cease
Full medical glossary




